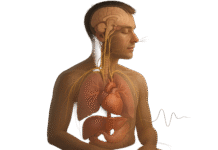
Gratitude isn’t only a “feel-good” idea—it’s linked to measurable shifts in sleep, cardiovascular tone, inflammation, and immune defenses. In plain terms, gratitude practices can support your body’s stress systems, promote better rest, and nudge key health behaviors that matter for immunity. In one sentence: gratitude influences physical health and immunity through stress reduction, improved sleep, autonomic balance, and downstream changes in inflammation and health behaviors, as shown in randomized and clinical studies.
Quick note: This article is educational and not a substitute for personal medical care. If you live with a medical condition, talk to your clinician before changing medications or care plans.
1. Calms the Stress Response (HPA Axis) to Protect Immune Balance
Gratitude helps downshift the body’s stress systems, which, when overactive, can suppress parts of immune defense and promote chronic inflammation. When stress is high, cortisol and sympathetic “fight-or-flight” activity can inhibit antibody production and skew immune signaling. Reviews of stress immunology consistently show that chronic stress dysregulates immune function; gratitude, as a positive affective state and practice, counters this by shifting attention and appraisals in ways that blunt reactivity. Emerging trials examining gratitude writing and gratitude meditation report lower heart rate during gratitude conditions versus “resentment” or neutral states, suggesting a calmer physiological set-point that’s friendlier to immunity.
1.1 Why it matters
- Chronic stress is linked to impaired vaccine responses and higher infection susceptibility; reducing stress supports more robust immune function.
- Gratitude practices cultivate positive affect, which correlates with healthier immune profiles. Carnegie Mellon University
1.2 How to do it (5–10 minutes)
- Set a daily 5-minute timer; write three specific things that went well and why.
- Add one “thank-you” text or voice note to someone who helped you today.
- Before sleep, reread what you wrote and notice one body signal of calm (e.g., softer shoulders).
Synthesis: By buffering stress physiology, gratitude removes a major brake on immune function while reinforcing a calmer baseline that carries over into sleep and daily recovery.
2. Improves Sleep—A Cornerstone of Antiviral Immunity
Better sleep is one of the most direct ways gratitude may support immunity. Trait gratitude predicts higher sleep quality and duration and less time to fall asleep, largely by shifting pre-sleep thoughts from rumination to positive reflections. Importantly, sleep doesn’t just feel good—it modifies your infection risk. Experiments exposing healthy adults to a cold virus found that shorter sleep and poorer efficiency in the prior weeks predicted a higher chance of getting sick; subsequent work with actigraphy confirmed that sleeping six hours or less sharply increased cold susceptibility. Gratitude’s effect on pre-sleep cognition is therefore a realistic lever for immune resilience. PMC
2.1 Mini checklist for tonight
- Stop screens 30–60 minutes before bed; write a “3 good things” list.
- Turn one good thing into a 30-second visualization.
- If a worry pops up, jot it on a “tomorrow” list and return to your gratitude page.
2.2 Numbers & guardrails
- In viral-challenge research, <7 hours sleep was associated with ~3–4× higher cold risk versus ≥7 hours. Aim for 7–9 hours where possible (as of August 2025).
Synthesis: Gratitude changes what’s on your mind at bedtime, which improves sleep continuity; better sleep, in turn, makes your immune system harder to knock over.
3. Supports Heart Health via Autonomic Balance and Blood Pressure
Cardiovascular and immune systems talk to each other through autonomic pathways. In a randomized study, a two-week gratitude intervention improved sleep and reduced diastolic blood pressure compared with active and no-treatment controls. Neuroimaging work shows lower heart rate during gratitude states versus resentment, consistent with increased parasympathetic (vagal) influence. Greater vagal activity—often indexed with heart rate variability (HRV)—is broadly associated with better stress recovery and inflammatory control. Together, these findings suggest that gratitude can tilt the nervous system toward “rest-and-digest,” which is good for both heart and immune function.
3.1 Practical steps
- Pair your gratitude journal with paced breathing (5–6 breaths/min) for 2–3 minutes to encourage vagal tone.
- After writing, sit quietly and re-experience one grateful moment; notice the natural pause after each exhale.
- Track resting heart rate or HRV trends with a wearable for 4–8 weeks to spot improvements.
3.2 Mini case
- In a small RCT, gratitude training in young women led to greater well-being and lower diastolic BP. While short and limited to one demographic, it demonstrates a plausible autonomic route for gratitude’s physical effects.
Synthesis: By nudging the autonomic nervous system toward parasympathetic dominance, gratitude can ease cardiovascular load—a shift that often travels with calmer inflammation and steadier immunity.
4. Lowers Inflammatory Biomarkers in Clinical Populations
Inflammation is a useful immune tool, but chronically high levels (e.g., CRP, IL-6, TNF-α) can be harmful. In patients with Stage B (asymptomatic) heart failure, eight weeks of gratitude journaling improved heart-related biomarkers and reduced circulating inflammatory markers compared with controls; related observational work found that higher dispositional gratitude correlated with lower inflammatory indices in the same patient population. While early and often small, these studies suggest gratitude can modulate systemic inflammation—especially when combined with standard medical care.
4.1 What the studies did
- Frequency: typically daily or most days for 6–8 weeks.
- Format: brief written entries focusing on specific events/people and why they mattered.
- Outcomes: changes in composite inflammatory indices; in some cases, HRV improved during writing sessions.
4.2 Guardrails
- These are adjuncts, not replacements, for clinical treatment. Discuss new practices with your clinician if you have cardiovascular disease or chronic inflammatory conditions.
Synthesis: Early clinical evidence indicates gratitude practices can move inflammatory needles in the right direction, complementing medical therapy in populations sensitive to inflammation.
5. Strengthens Health Behaviors That Defend Immunity
One understated pathway: gratitude makes health behaviors easier to do. In classic experiments, people assigned to weekly “count your blessings” sessions reported fewer physical symptoms and nearly 1.5 more hours of exercise per week than those who logged hassles. Later analyses show that grateful adults often report better sleep routines, greater self-care, and stronger social support—all predictors of healthier immune profiles. In other words, gratitude doesn’t have to act directly on cells to help your immunity; it can reshape the daily inputs (movement, rest, adherence) that your immune system depends on. PMC
5.1 Behavior nudges to try
- After journaling, schedule tomorrow’s walk or workout (even 20 minutes counts).
- Write one line about how a future “you” benefits from today’s small action.
- Use a simple tracker (✓ marks) for sleep, movement, and gratitude across 30 days.
5.2 Why it sticks
- Positive affect broadens attention and increases approach-oriented behaviors, making “healthy” actions feel more doable and rewarding, not just obligatory. ScienceDirect
Synthesis: Gratitude improves the odds you’ll do the basics—move, sleep, and care for yourself—which cumulatively lift immune resilience.
6. Reduces Pain and Physical Symptom Burden
Pain and immune signaling are intertwined. Meta-analytic and clinical findings suggest gratitude practices reduce psychological distress and may lower perceived pain in some chronic conditions. Observational work and small trials show that individuals with higher gratitude report fewer daily physical symptoms; early studies in fibromyalgia point to reduced symptom severity and better sleep patterns when gratitude is cultivated alongside standard care. While mechanisms are still being clarified (e.g., reduced catastrophizing, improved sleep, social buffering), the direction is promising—and meaningful for quality of life.
6.1 Tools/Examples
- Turn a pain flare into a “micro-gratitude scan”: name three supports (a person, a tool, a coping skill) aiding you right now.
- Pair gratitude with diaphragmatic breathing during discomfort to reduce sympathetic arousal.
- For chronic pain, consider integrating gratitude prompts into CBT or ACT frameworks.
6.2 Common mistakes
- Using gratitude to deny or minimize pain (“toxic positivity”).
- Writing generic entries; specificity strengthens the analgesic effect.
Synthesis: By easing distress and improving sleep and coping, gratitude can shrink the day-to-day footprint of pain and somatic complaints, indirectly supporting immune balance.
7. May Enhance Vaccine Responses Through Positive Affect
A robust literature links positive mood with stronger antibody responses to vaccines. For example, higher dispositional positive affect predicted a greater antibody response to the hepatitis B vaccine, and positive mood on the day of influenza vaccination correlated with better antibody titers in older adults. Gratitude reliably increases positive affect, making it a plausible (and safe) way to “prime” your internal environment before vaccination—especially when combined with good sleep. While gratitude-specific vaccine trials are limited, the affect→immunity pathway is consistent and clinically relevant. PMC
7.1 Pre-vaccine mini-protocol (evidence-informed)
- Two nights before: 7–9 hours of sleep; write three gratitudes and why each mattered.
- Day of vaccination: 3-minute gratitude visualization; send one sincere thank-you.
- Post-shot: hydrate, rest, and keep sleep steady for a week.
7.2 Region notes
- If you’re in a setting with limited vaccine access, the biggest win is still getting vaccinated. Gratitude is an adjunct, not an alternative.
Synthesis: Positive affect is a small but real lever for vaccine responses; gratitude is a practical way to turn that lever.
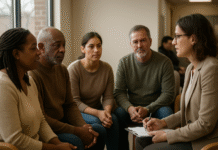
8. Builds Social Connection—A Known Immune Buffer
Immune function is shaped by social context. Recent reviews highlight how prosocial behavior and social support map onto healthier immune profiles and better outcomes. Gratitude—felt and expressed—reliably strengthens relationships by increasing perceived warmth, reciprocity, and support. That support, in turn, is linked with reduced inflammation and better immune regulation under stress. In short: gratitude helps you help your immune system by improving the relational environment it lives in.
8.1 How to operationalize it
- Make “gratitude rounds” weekly: identify two people to thank for something specific.
- Use the “because” rule in thank-yous (“because you stayed late, I could rest”).
- Rotate between text, voice note, and in-person thanks to keep it genuine.
8.2 Mini example
- Workplace trial idea: team starts meetings with one quick acknowledgment. Track informal support and sick-day usage over a quarter to check for trends (observational).
Synthesis: By amplifying social support—one of the most reliable immune buffers—gratitude changes not just how you feel, but the network that helps you stay healthy. ScienceDirect
9. A Safe, Measurable Regimen to Translate Gratitude Into Health Gains
To move from “nice idea” to body-level change, make gratitude a repeatable routine with simple metrics. Many of the strongest effects in studies come from 2–8 weeks of brief, regular practice. Pair gratitude with sleep hygiene, movement, and stress skills to compound benefits. Track outcomes you care about (sleep, resting heart rate, step counts, medication adherence) and look for steady, not dramatic, shifts—these are the type most associated with durable immunity and lower inflammation in broader literature.
9.1 Weekly plan (8 weeks)
- Mon/Wed/Fri: 5-minute “3 good things” + 2 minutes of slow breathing.
- Tue/Thu: One expression of thanks (message or in person).
- Sat/Sun: 10-minute longer entry (one story + why it mattered).
- Daily: 7–9 hours sleep target; 20–30 minutes of movement.
9.2 What to track (and why)
- Sleep duration/quality (immune readiness).
- Resting HR/HRV (autonomic balance).
- Symptom check (aches, fatigue) weekly for trends.
- Adherence (meds, appointments) if relevant.
Synthesis: A light-lift, repeatable protocol—combined with core health behaviors—turns gratitude from an intention into an immune-supportive habit loop grounded in research timelines.
FAQs
1) How fast can I expect physical changes from gratitude practice?
Many trials run 2–8 weeks and observe improvements in sleep, mood, and sometimes physiological markers within that window. Biomarker shifts (e.g., inflammation) are typically small and best interpreted alongside standard care. Stay consistent for at least a month before judging results.
2) Is gratitude enough to “boost” my immune system?
No single practice “boosts” immunity across the board. Gratitude is best viewed as a support: it improves sleep and stress regulation, which are foundational for immune function, and it helps you follow through on healthy behaviors. Pair it with vaccines, good sleep, movement, and medical care.
3) Which gratitude exercise has the most evidence?
Brief writing (“counting blessings” or gratitude journaling) has been widely studied and shows benefits for physical symptoms, exercise, and well-being; clinical studies in heart failure used daily journaling over eight weeks. Expressing thanks to others adds a social-support boost.
4) Can gratitude lower blood pressure?
A two-week randomized trial in young women found reductions in diastolic pressure versus controls. Effects vary by person and aren’t a replacement for antihypertensives, but they suggest autonomic pathways (vagal tone) may be involved.
5) Does gratitude really help me sleep?
Yes—trait gratitude predicts better sleep quality and duration, partly by shifting pre-sleep thoughts from worry to positive reflections. Combining gratitude writing with basic sleep hygiene is a practical way to use this pathway.
6) Is there evidence gratitude affects inflammation?
Pilot clinical work in asymptomatic heart failure shows reduced inflammatory markers after eight weeks of gratitude journaling; observational data in the same population links higher gratitude with lower inflammatory indices. Larger, diverse trials are needed.
7) Could gratitude improve my response to vaccines?
Direct gratitude-specific vaccine trials are scarce, but positive affect (which gratitude increases) has been associated with stronger antibody responses to vaccines like hepatitis B and influenza. Consider a pre-vaccine gratitude routine as an adjunct.
8) I live with chronic pain—how might gratitude help?
Studies in chronic pain populations (e.g., fibromyalgia) suggest gratitude relates to lower symptom severity, better sleep, and improved well-being. Use gratitude alongside evidence-based pain management and avoid minimizing your experience. MDPI
9) How do I keep gratitude from feeling fake?
Be specific and honest. Thank the person or moment and explain why it mattered. If the day was hard, name one small support that helped. Forced positivity backfires; specificity builds authenticity. (General practical guidance aligned with intervention protocols.) Greater Good
10) What’s a realistic “dose” per week?
In research, brief entries 3–7 days/week over 6–8 weeks are common. If you’re starting out, aim for 3–4 days/week and scale as it becomes natural.
Conclusion
Gratitude’s promise for physical health isn’t magic—it’s mechanics. By easing stress physiology, improving sleep, and nudging the autonomic nervous system toward balance, gratitude creates conditions where immune defenses work more smoothly and inflammation stays in check. Add the social-support boost and the way gratitude makes healthy behaviors more likely, and you get a compounding effect: modest, durable gains that matter in real life. The most important move is to make gratitude repeatable—5–10 minutes most days, plus a small expression of thanks to someone else. Track sleep, resting heart rate, and symptom trends for eight weeks to see your own data. Then keep what works.
Start tonight: write three specifics you’re grateful for, add one thank-you, and get seven hours of sleep. Your body—and your immune system—will thank you for it.
References
- Redwine, L. S., et al. “A Pilot Randomized Study of a Gratitude Journaling Intervention on Heart Rate Variability and Inflammatory Biomarkers in Patients with Stage B Heart Failure.” Psychosomatic Medicine, 2016. PMC
- Mills, P. J., et al. “The Role of Gratitude in Spiritual Well-Being in Asymptomatic Heart Failure Patients.” Spirituality in Clinical Practice, 2015. PubMed
- Jackowska, M., et al. “The Impact of a Brief Gratitude Intervention on Subjective Well-Being, Biology and Sleep.” Journal of Health Psychology, 2016. PubMed
- Wood, A. M., et al. “Gratitude Influences Sleep Through the Mechanism of Pre-Sleep Cognitions.” Journal of Psychosomatic Research, 2009. PubMed
- Cohen, S., et al. “Sleep Habits and Susceptibility to the Common Cold.” Archives of Internal Medicine, 2009. JAMA Network
- Prather, A. A., et al. “Behaviorally Assessed Sleep and Susceptibility to the Common Cold.” Sleep, 2015. PMC
- Kyeong, S., et al. “Effects of Gratitude Meditation on Neural Network Functional Connectivity and Brain-Heart Coupling.” Scientific Reports, 2017. Nature
- Laborde, S., et al. “Heart Rate Variability and Cardiac Vagal Tone in Psychophysiological Research—Practical Recommendations.” Frontiers in Psychology, 2017. https://www.frontiersin.org/articles/10.3389/fpsyg.2017.00213/full Frontiers
- Emmons, R. A., & McCullough, M. E. “Counting Blessings Versus Burdens: An Experimental Investigation of Gratitude and Subjective Well-Being in Daily Life.” Journal of Personality and Social Psychology, 2003. Emmons Faculty Site
- Alotiby, A. “Immunology of Stress: A Review.” International Journal of Molecular Sciences, 2024. PMC
- Marsland, A. L., et al. “Trait Positive Affect and Antibody Response to Hepatitis B Vaccination.” Brain, Behavior, and Immunity, 2006. PubMed
- Ayling, K., et al. “Positive Mood on the Day of Influenza Vaccination Predicts Vaccine Effectiveness.” Brain, Behavior, and Immunity, 2018. ScienceDirect
- Wang, X., et al. “The Impact of Gratitude Interventions on Patients with Cardiovascular Disease.” Frontiers in Psychology, 2023. Frontiers
- American College of Cardiology. “FEEL Study: Spirituality, Gratitude and Hypertension.” ACC.org News, April 7, 2024. acc.org