Your circadian rhythm is your internal 24-hour timekeeping system that coordinates sleep, hormones, body temperature, metabolism, and alertness. In simple terms, it’s how your brain and body anticipate day and night so you feel sleepy at night and alert in the morning. When that timing is aligned with your life, you sleep better, think more clearly, and feel steadier energy. When it’s off—through late-night light, irregular schedules, jet lag, or shift work—sleep quality, mood, and metabolic markers tend to suffer. This guide distills the science into 9 practical principles you can use to understand and tune your clock.
Snapshot answer: Your internal clock is set primarily by light (especially morning daylight), supported by regular sleep times, meals, activity, and temperature cues. Get bright light soon after waking, dim light for 3+ hours before bed, anchor a consistent sleep window, time meals earlier, move daily, and use strategic tools (e.g., melatonin for jet lag) sparingly and at the right time.
1. The Master Clock and Clock Genes: How Your Body Keeps Time
Your circadian system is organized around a master pacemaker—the suprachiasmatic nucleus (SCN)—a tiny bundle of ~20,000 neurons in the hypothalamus that synchronizes clocks across your body. The SCN receives direct light information from the eyes and then coordinates rhythms in hormones (like melatonin and cortisol), core body temperature, and behavior. Inside nearly every cell, clock genes (including CLOCK, BMAL1, PER, and CRY) form self-sustaining feedback loops that generate ~24-hour oscillations. In controlled conditions, the human clock “free-runs” just longer than 24 hours on average (≈24.18 hours), so daily cues are essential to keep you aligned to solar time. This networked design—SCN at the top, peripheral clocks throughout organs—explains why consistent daily habits and light exposure are so powerful: they retune the whole orchestra, not just one instrument.
1.1 Why it matters
A synchronized clock improves sleep timing, metabolic efficiency, and cognitive performance. Misalignment (e.g., inconsistent bedtimes, late-night lighting, erratic meals) increases sleepiness at the wrong times and can degrade mood and metabolic health. Knowing there’s one master conductor (SCN) helps you focus on the highest-leverage cue: light timing.
1.2 How it works (quick primer)
- The SCN receives light signals via the retinohypothalamic tract from specialized retinal cells.
- In cells, clock genes create ~24-hour cycles through transcription–translation feedback.
- The SCN sends timing signals (neural and hormonal) to align peripheral clocks (liver, pancreas, muscle, fat).
- Without daily cues, your internal “day” drifts later by ~0.2 hours/day on average, reinforcing the need for timed light, meals, and activity.
1.3 Mini-checklist
- Prioritize morning daylight to “pin” the SCN each day.
- Keep a consistent sleep-wake window (±30–60 minutes).
- Avoid irregular, late-night light and meals that desynchronize organ clocks.
Bottom line: Treat the SCN like a conductor: give it strong, consistent morning light and predictable daily timing so every tissue plays in time.
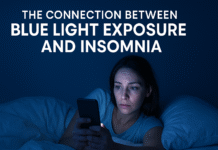
2. Light Is the Strongest Zeitgeber: Timing, Spectrum, and Dose
Light is your clock’s loudest cue (“zeitgeber”). Specialized retinal cells—ipRGCs containing melanopsin—are most sensitive to blue-cyan light around ~480 nm. Morning light (especially daylight) advances the clock so you feel sleepy earlier that night; evening light tends to delay it, pushing sleep later. Beyond timing, intensity, spectrum, and duration matter: brighter, bluer, and longer exposures have stronger effects. As of August 2025, consensus guidance using melanopic equivalent daylight illuminance (melanopic EDI) suggests aiming for ≥250 melanopic lux in daytime, ≤10 melanopic lux during the 3 hours pre-bed, and ≤1 melanopic lux during sleep. Practically, that means lots of outdoor light shortly after waking and progressively warmer, dimmer lighting at night.
2.1 Numbers & guardrails
- Advance window: Morning/early-day light (especially after your core-body-temp minimum) nudges your rhythm earlier.
- Delay window: Evening light delays your clock; even typical room light (~50–200 lux) can suppress melatonin and shift timing.
- Melanopic EDI targets: ≥250 (day), ≤10 (evening), ≤1 (sleep). Use warmer bulbs and dimmers at night.
2.2 How to do it (everyday playbook)
- Morning: 30–60 minutes outside within 1–2 hours of waking (even through clouds).
- Workday: Sit near a window or take light breaks; consider a light box if daylight is limited.
- Evening: Dim lights 3+ hours before bed; use warm-tone lamps; reduce overhead lighting.
- Screens: Turn on night modes, lower brightness, and increase font size to avoid straining into bright light.
- Bedroom: Aim for near-dark—cover LEDs, use blackout curtains; if needed, a low, warm nightlight.
Bottom line: Light is medicine for your clock. Dose it bright and early; taper it low and warm at night.
3. Sleep Pressure vs. the Clock: The Two-Process Model You Can Use
Your sleep is governed by two processes. Process S (homeostatic sleep pressure) builds the longer you’re awake and dissipates during sleep; Process C (circadian) times when sleep is most likely and consolidated. You fall asleep most easily when pressure is high and the circadian signal allows it. Napping late, sleeping in far past your usual time, or blasting bright light late can uncouple S and C: you won’t feel sleepy at night, and mornings feel brutal. The strategy is to align them—build enough sleep pressure during the day and time your light so your circadian gate opens at bedtime.
3.1 Practical cues
- Keep rise time consistent; it’s the anchor that sets both S and C.
- Nap smart: if you must, 10–30 minutes, before mid-afternoon.
- Get daylight + activity to build healthy pressure; avoid long, late naps.
3.2 Common mistakes
- Weekend drift: sleeping in 2–3+ hours creates a “Monday jet lag.”
- Late caffeine: pushes sleep pressure off and masks sleepiness.
- Bright late-evening light: delays Process C, making bedtime feel “too early.”
Bottom line: Align the “need” to sleep (S) with the “permission” to sleep (C). Consistent mornings, smart light, and well-timed naps do most of the work.
4. Hormones and Temperature: Melatonin, Cortisol, and Core Body Temperature
Your clock choreographs daily rises and falls in key signals. Melatonin rises in dim light about 2–3 hours before your habitual bedtime (the DLMO), peaks in the early morning, then falls with daytime light. Cortisol typically peaks within the first hour after waking (the CAR) and declines across the day. Core body temperature (CBT) is highest in the evening and nadir in the second half of the night/very early morning; many performance measures mirror CBT. When these curves are out of sync with sleep timing, you feel “wired but tired” at night and sluggish in the morning. Protecting darkness before bed (and darkness during sleep) stabilizes melatonin; bright daytime light and morning movement support the cortisol profile.
4.1 Why it matters
- DLMO is the most reliable clinical marker of your clock’s phase.
- Cortisol & CBT shape alertness windows; mismatches reduce sleep quality and daytime performance.
- Evening room light (even <200 lux) can delay melatonin onset and shorten its duration.
4.2 Tools/Examples
- For stubborn timing issues, clinicians may measure salivary DLMO with at-home kits.
- If you wake too early, dim late-evening light less and favor light exposure later in the morning; if you fall asleep too late, push morning light earlier and dim earlier at night.
Bottom line: Darkness before and during sleep isn’t optional—it’s a hormonal signal. Daylight after waking is its partner.
5. Chronotype & Social Jet Lag: Work With Your Biological Preference
Chronotype is your preferred timing (lark ↔ owl), influenced by genetics, age, and light history. Teens trend later; older adults trend earlier. Social jet lag is the gap between your biological time and social schedule, often measured as the difference in the midpoint of sleep on workdays vs. free days. Large gaps (≥1–2 hours) correlate with higher fatigue, worse mood, and, in some studies, higher BMI or metabolic risk. The goal isn’t to force a lark’s schedule on an owl; it’s to reduce misalignment with smarter light, anchors, and expectations.
5.1 How to measure
- Track bed/wake times for 7–14 days; compute mid-sleep on workdays vs. free days.
- Use validated questionnaires (e.g., MCTQ); adjust for weekend oversleep.
- Cross-check your energy and focus peaks with timing data.
5.2 Guardrails to shrink the gap
- Fix your wake time within ~1 hour all week.
- Add earlier morning light (and earlier dimming) if you’re consistently late.
- Keep weekend drift to ≤1 hour; if you must shift, do it gradually (15–30 minutes/day).
Bottom line: Respect your chronotype but smooth the edges. Small, consistent timing moves beat occasional extreme resets.
6. Meal Timing and Peripheral Clocks: Feed the Right Time
While light sets the SCN, meals help set peripheral clocks in the liver, pancreas, and gut. Eating very late can desynchronize metabolic rhythms from your brain’s clock, impairing glucose handling and GI comfort at night. Early time-restricted eating (eTRE)—keeping meals within an 8–12-hour daytime window and finishing 2–3 hours before bed—has shown benefits in small trials (e.g., insulin sensitivity, blood pressure), especially when the window skews earlier in the day. You don’t need to be perfect; you do need to be predictable: similarly timed meals most days guide peripheral clocks.
6.1 How to do it
- Pick a consistent window (e.g., 08:00–18:00) on workdays; loosen by ≤1 hour on weekends.
- Front-load calories earlier; make late dinners lighter and earlier.
- Avoid large meals in the 3 hours pre-bed to reduce reflux and nocturnal arousals.
6.2 Mini-checklist
- Hydrate and eat breakfast/brunch on time to start the daytime program.
- If you exercise late, choose lighter, protein-forward post-workout meals.
- Travel days: shift mealtimes toward destination time on the plane.
Bottom line: Regular, earlier meals align organ clocks with your sleep clock. Predictability beats perfection.
7. Movement as a Secondary Zeitgeber: Time Your Exercise
Exercise can shift the clock modestly and powerfully improves sleep depth and quality. Morning and mid-day exercise generally favors advancing your rhythm (sleep earlier), while late-evening vigorous exercise can delay timing for some people—though the effect varies by intensity and individual sensitivity. Compared with light, exercise is a weaker zeitgeber, but it’s still useful: combine morning light + morning activity for the strongest advance; use late-afternoon/early-evening workouts if you need a small delay (e.g., habitual early awakening).
7.1 Numbers & notes
- Aim for 150–300 minutes/week of moderate aerobic movement plus 2–3 strength sessions.
- Finish vigorous sessions ≥2–3 hours before bed if you’re sensitive to late exercise.
- Pair movement with outdoor light whenever possible.
7.2 Practical templates
- Advance plan: 20–40 min brisk walk or jog within 2 hours of waking + daylight.
- Delay plan: If nights feel too early, try early-evening training ending by ~3 hours pre-bed, dim late light responsibly.
Bottom line: Exercise helps, especially when paired with the right light. Time it to nudge your clock in the direction you want.
8. Jet Lag and Shift Work: Managing Misalignment
Crossing time zones and working nights/rotating shifts create a mismatch between your internal time and local time. Most people adapt faster going west (delays) than east (advances). Roughly, expect adaptation on the order of ~1–1.5 hours/day depending on direction and strategy. Evidence-based tools include timed light exposure/avoidance, timed melatonin (often 0.5–1 mg for phase shifting), sleep scheduling, and short-term use of stimulants/hypnotics under medical guidance. The key is timing—mistimed light or melatonin can make jet lag worse.
8.1 How to do it (quick planner)
- Pre-flight: Shift sleep 30–60 minutes/day toward destination for 2–3 days; adjust meal and light timing too.
- In flight: Set your watch to destination; manage light (shade up/down, sunglasses) accordingly; hydrate.
- At destination: Use morning daylight for eastward trips and late-afternoon/evening light for westward trips; avoid light at the “wrong” circadian times (dark glasses, hat). Consider 0.5–1 mg melatonin at the new biological evening for a few days.
8.2 Shift work notes
- On permanent nights, anchor a consistent post-shift sleep period and use bright light at work/darkness at home (blue-blocking glasses on commute).
- On rotating shifts, use strategic naps, caffeine early in shift only, and blackout conditions for day sleep.
Bottom line: Plan your light and melatonin like a medication—dose and timing matter more than quantity.
9. Reset and Protect: A 14-Day Circadian Tune-Up
When you need a reset—after travel, an all-nighter, or months of drift—run a structured two-week protocol. The objective is to flood mornings with daylight, lock your anchor times, and drain evening light. Expect meaningful improvements in sleep latency, continuity, and morning alertness within 7–14 days.
9.1 The plan
- Wake time: Fix a wake time you can keep 7 days/week (±30–60 min).
- Morning light: 30–60 minutes outdoors within 2 hours of waking; add another light break near midday.
- Activity: Move daily; schedule strength or cardio on most days.
- Caffeine: Last dose ≥8 hours before bed; none after mid-afternoon if sensitive.
- Meals: Stable daytime window; finish 2–3 hours pre-bed.
- Evening: Dim lights 3+ hours before bed; warm lamps only; reduce screens or use night modes.
- Bedroom: Make it dark, cool (~17–19°C / 63–66°F), and quiet.
9.2 Case example (evening type drifting late)
- Target: Shift bedtime from 1:00 a.m. → 11:00 p.m. over 14 days.
- Steps: Wake 7:00 a.m. daily; 45 minutes outside by 7:30–8:15; exercise at 8:30–9:00 three days/week; dim lights from 8:00 p.m.; no screens past 9:30; bed 11:00.
- Result: Sleep onset pulls earlier, morning alertness improves, weekend drift shrinks.
Bottom line: Consistency plus morning light is the lever. Two weeks of disciplined timing usually earns you a stable rhythm.
FAQs
1) What exactly is a circadian rhythm?
It’s your body’s internal, roughly 24-hour program that coordinates sleep, hormones, temperature, metabolism, and behavior with the cycle of day and night. A synchronized rhythm means you’re sleepy at night, alert by day, and your organs run on schedule. When it’s misaligned (late light, irregular sleep, travel, shift work), sleep and energy suffer and metabolic markers can drift.
2) How much light is “enough” in the morning?
Daylight is best. As a rule of thumb, spend 30–60 minutes outdoors within 1–2 hours of waking. Indoors, standard lighting often provides too little circadian stimulus; if you can’t get outside, sit by a bright window or consider a quality light box. At night, dim and warm the lighting—your clock cares about both timing and brightness/spectrum.
3) Do blue-light–blocking glasses fix everything?
They can help reduce melanopsin-stimulating wavelengths at night, but they’re not magic. Even with glasses, bright light can delay your clock. The bigger wins are dimming lights, using warmer bulbs, and reducing screen time in the 3 hours before bed. In the day, you want the opposite: more bright light, ideally outdoors.
4) Are naps bad for circadian rhythm?
Short, early-day naps (10–30 minutes) can boost alertness without disrupting night sleep. Long or late naps can reduce homeostatic sleep pressure and push bedtime later. If you struggle to fall asleep at night, cap naps and keep them before mid-afternoon.
5) When should I stop caffeine?
Caffeine’s half-life averages around 5 hours, but sensitivity varies. As a conservative rule, finish caffeine 8 hours before your target bedtime; caffeine later than mid-afternoon often delays sleep onset and lightens sleep depth for sensitive people.
6) How do I find my chronotype without a lab?
Track your natural sleep times for 1–2 weeks when you’re free to choose your schedule and compute your midpoint of sleep on those free days (adjust for catch-up oversleep). That midpoint is a decent proxy for chronotype; there are validated questionnaires that do this too.
7) Is melatonin safe to take nightly?
Low-dose melatonin can help shift timing or support sleep during travel, but it’s a hormone and timing matters. Many people don’t need nightly melatonin if they manage light well. If you use it for jet lag or circadian issues, 0.5–1 mg at the right clock time is commonly used for shifting; avoid high doses unless guided by a clinician.
8) Should I try time-restricted eating for my clock?
Keeping meals in a consistent daytime window and finishing 2–3 hours before bed supports metabolic rhythms. Early windows (earlier, not smaller) tend to align better with the clock. You don’t have to be strict daily; predictable timing most days helps.
9) How long does it take to “reset” after a late night or all-nighter?
Expect 1–3 days of disciplined light and timing to feel normal again. Use strong morning daylight, stick to your wake time, and dim evenings. Avoid trying to “sleep until noon”—it usually prolongs the drift.
10) What’s the difference between circadian rhythm and sleep duration?
Duration is how long you sleep; circadian rhythm is when your body wants to sleep and wake. You can get 8 hours at the “wrong” time and still feel off because hormones, temperature, and alertness curves are misaligned. Best outcomes combine enough sleep and aligned timing.
Conclusion
Your internal clock is not a mysterious black box; it’s a trainable system with clear inputs. Light is the master lever: bright and early to set the day, dim and warm to invite the night. Consistency is the amplifier: a steady wake time, a predictable meal window, and routine movement keep peripheral clocks in sync with the SCN. Context is the fine-tuner: adjust exercise timing, caffeine cutoffs, and evening light to fit your chronotype and goals. Whether you’re recovering from jet lag, stabilizing a shifting work schedule, or just wanting better mornings, a 14-day tune-up with anchored wake time, morning daylight, and low-light evenings can reset your rhythm. Start tomorrow morning with 30–60 minutes of daylight, set your caffeine curfew, and dim your evenings—your clock will thank you.
CTA: Give yourself 14 days of bright mornings and dim evenings—track your sleep and see the difference.
References
- Circadian Rhythms (Fact Sheet) — National Institute of General Medical Sciences (NIGMS), May 20, 2025. NIGMS
- The 2017 Nobel Prize in Physiology or Medicine — Press Release — Nobel Prize Outreach, Oct 2, 2017. NobelPrize.org
- Stability, Precision, and Near-24-Hour Period of the Human Circadian Pacemaker — C.A. Czeisler et al., Science, June 25, 1999. PubMed
- Recommendations for Daytime, Evening, and Nighttime Indoor Light Exposure to Best Support Physiology, Sleep, and Wakefulness in Healthy Adults — T.M. Brown et al., PLOS Biology, 2022. PMC
- Exposure to Room Light Before Bedtime Suppresses Melatonin Onset and Shortens Melatonin Duration in Humans — J.J. Gooley et al., J Clin Endocrinol Metab, 2011. PubMed
- Measuring and Using Light in the Melanopsin Age — R.J. Lucas et al., Trends in Neurosciences, 2014. PMC
- The Two-Process Model of Sleep Regulation: A Reappraisal — A. Borbély et al., Journal of Sleep Research, 2016. Centre for Chronobiology
- The Dim Light Melatonin Onset Across Ages, Methodologies, and Populations — D.J. Kennaway, Sleep, 2023. PMC
- The Intrinsic Near-24-h Pacemaker Period Determines Limits of Entrainment — K.P. Wright Jr. et al., PNAS, 2001. PMC
- Jet Lag Disorder (CDC Yellow Book, 2026 Edition) — Centers for Disease Control and Prevention, Apr 23, 2025. CDC
- Human Phase Response Curve to Exercise (Meta-analysis/Experiment) — M.H. Youngstedt et al., PLOS ONE, 2019. https://journals.plos.org/plosone/article PubMed
- ipRGCs in Humans — A Review — L.S. Mure, Current Opinion in Physiology, 2021. https://www.sciencedirect.com/science/article/pii/S2468867319302763 PMC
- Cortisol Circadian Timekeeping and Glucocorticoids — J.P. O’Byrne & A.V. Chernyshev, Endocrine Reviews, 2021. https://pubmed.ncbi.nlm.nih.gov/34449255/ PMC
- Time-Restricted Eating: A Systematic Review — M. Lundell et al., Nutrients, 2023. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10345971/ PMC
- Spectral Sensitivity of Human Circadian Phase Resetting — M.A. St. Hilaire et al., PNAS, 2022. PNAS