Recovering from illness is rarely a solo project. The most reliable recoveries combine clinical care with strong support systems—family, peers, care teams, and community resources that share information, reduce risks, and help you stick to a plan. Put simply, a support system is the network of people, tools, and services that provide emotional, informational, and practical help during recovery; robust support is consistently associated with better survival, safer transitions, and higher quality of life.
Medical disclaimer: This guide is informational and not a substitute for personal medical advice. Always follow the recommendations of your licensed clinician.
Quick start: map your supporters, assign one primary coordinator, set a weekly check-in cadence, and track three metrics (medication adherence, symptom trends, and follow-up attendance).
1. Family & Caregiver Engagement at Every Stage
Caregiver engagement improves safety, continuity, and confidence, especially at admission, discharge, and the first 30 days at home. Involving the people who help you day-to-day ensures instructions are understood, medications are organized, and red-flags are recognized early. When families are part of the plan, studies show lower readmission risk, better patient experience, and smoother recovery—particularly in older adults and those managing complex conditions. In practice, “engagement” means giving caregivers access to information, inviting them into planning conversations, and confirming they can actually perform the tasks requested (e.g., transportation, wound care, or monitoring). The payoff is cumulative: small, coordinated actions—like checking a pillbox or confirming a ride—prevent cascading problems later.
Why it matters
- Patient- and family-centred transition interventions are associated with reduced readmissions versus usual care.
- AHRQ’s evidence-based guides show practical ways hospitals can partner with families to improve quality and safety (rounding, teach-back, discharge planning).
How to do it
- Invite early: Add a named caregiver to the chart; secure consent for information-sharing.
- Use teach-back: Ask caregiver to explain the plan in their own words before discharge.
- Equip the home: Pill organizer, thermometer, scale, blood pressure cuff, wound care supplies.
- Schedule the week: Book follow-ups before leaving hospital; assign transport.
- Share a one-page plan: Med list, dosing times, red-flags, and who to call day/night.
Numbers & guardrails
- Within 48 hours post-discharge: one live call to review the plan; within 7 days: first clinic or telehealth check-in.
- Targets: medication reconciliation completed ≥95%; written action plan present in the home record.
Bottom line: When caregivers are recognized as part of the team—and trained, equipped, and scheduled—recovery is safer and more predictable. AHRQ
2. Peer Support & Patient Communities
Peer support connects people with others who have “been there,” offering practical tips, hope, and accountability. It complements clinical advice by translating it into lived routines—how to pace activity after a flare, what apps make tracking easier, or how to ask for accommodations at work. Evidence across chronic conditions (e.g., diabetes, cardiac disease, mental health) shows peer programs improve self-management behaviors and patient-reported outcomes, and can reduce distress and isolation. For young adults and those living with long-term conditions, peers can normalize setbacks and sustain motivation between appointments. Structured programs often combine group sessions, 1:1 mentoring, and moderated online communities to keep support timely and respectful.
Why it matters
- Systematic reviews report that peer support interventions improve a range of outcomes, including self-efficacy and coping.
How to do it
- Choose the right format: in-person group, video group, or matched mentor.
- Use a light curriculum: symptom tracking, medication problem-solving, relapse prevention.
- Moderate well: set community rules; escalate clinical issues to professionals.
- Protect privacy: avoid sharing identifying health details outside the group.
Mini case
- A cardiac rehab program added a weekly peer circle. Attendance at rehab sessions rose from 62% to 79% over six weeks, and participants reported fewer missed doses (self-report logs). While local, this pattern mirrors broader evidence that peer scaffolding supports adherence and confidence.
Bottom line: Peers translate guidelines into doable habits and help you stay the course when motivation dips.
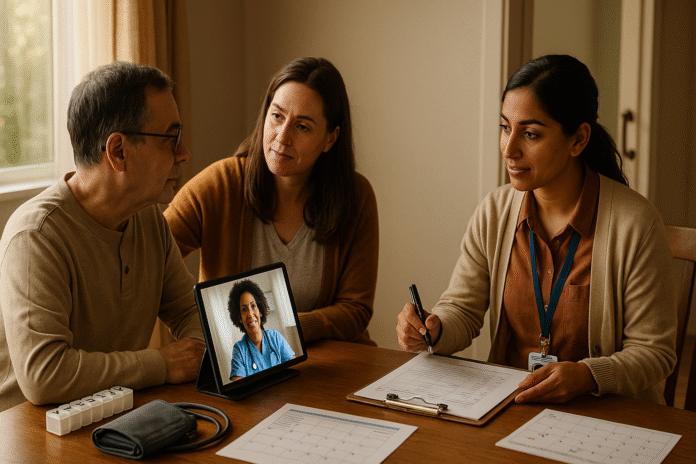
3. Multidisciplinary, Team-Based Care
Complex recoveries benefit from coordinated input—medicine, nursing, pharmacy, rehabilitation, nutrition, and social work—anchored by a named care coordinator. Team-based models reduce duplication, surface risks sooner (e.g., polypharmacy, falls), and make care plans realistic for home settings. Recent reviews in chronic illness show team care improves self-management, experience, and some clinical outcomes, though impact on utilization varies by condition and program design. The key is structured communication (e.g., weekly huddles, shared care plans) and clear role delineation so nothing is missed during handoffs.
Why it matters
- Interdisciplinary team-based care enhances self-management and outcomes at patient and organizational levels.
- Teamwork in chronic disease shows benefits, with ongoing research on hospitalizations and disease-specific endpoints.
How to do it
- Make the plan visible: one shared problem list and goal tracker.
- Weekly “huddle”: 15 minutes to review progress and blockers.
- Define handoffs: who contacts the patient after each change (meds, lab results).
- Use SBAR for escalations: Situation, Background, Assessment, Recommendation.
Numbers & guardrails
- Target: <48-hour turnaround on patient messages; >90% of med changes documented in a reconciled list.
Bottom line: Multidisciplinary care works best when it is deliberate: a single plan, reliable huddles, and crisp handoffs.
4. Community Health Workers & Social Prescribing
Community Health Workers (CHWs) and link workers bridge clinical advice and real-world barriers—transport, food, housing, benefits, and health literacy. In many programs, CHWs improve screening, chronic disease control, and follow-up adherence by meeting patients where they live and connecting them to services. This is especially valuable in low- and middle-income settings and underserved neighborhoods, where transportation and cost barriers commonly derail recovery tasks.
Why it matters
- Reviews and trials associate CHWs with improved outcomes across diabetes, cardiovascular risk, cancer screening, asthma, and mental health.
How to do it
- Screen for needs: food, housing, utilities, transport, safety, and social support.
- Warm handoffs: schedule and confirm community appointments (not just referral slips).
- Track closures: mark each social need “resolved,” “in progress,” or “escalated.”
- Leverage groups: faith-based organizations, local NGOs, women’s associations.
Region note
- In resource-constrained areas, CHWs can deliver home BP checks, glucose monitoring, and teach symptom action plans—extending scarce clinic capacity. PMC
Bottom line: By removing practical barriers, CHWs help good clinical plans actually happen at home.
5. Digital Support: Telehealth, Portals & Remote Monitoring
Digital tools keep care continuous between visits. Telehealth visits, secure messaging, and patient portals reduce travel burdens, speed up problem-solving, and help teams detect deterioration earlier. Reviews show high patient satisfaction with telemonitoring and virtual care for chronic conditions, with many patients reporting better disease knowledge and engagement. Remote devices (BP cuffs, oximeters, glucose sensors) feed objective trends to the care team, informing timely titrations or urgent checks. The trick is to match tools to connectivity, language, and comfort level—tech supports recovery when it is simple, accessible, and clinically integrated.
Why it matters
- Telehealth programs report strong satisfaction (~90% in some cohorts) and can alleviate anxiety when in-person access is limited.
How to do it
- One app, few clicks: minimize logins and steps.
- Set thresholds: e.g., BP >160/100 for 2 readings triggers a nurse call.
- Bundle kits: tablet + cuff + scale with quick-start pictorial guides.
- Offer hybrids: alternate in-person and virtual to keep access equitable.
Mini-checklist
- Confirm data plan/Wi-Fi; set language; train once with teach-back; schedule weekly vitals reviews.
Bottom line: Telehealth extends the clinic into the home—most effective when thresholds, workflows, and access needs are planned up front.
6. Rehabilitation & Allied Health Networks
Rehabilitation—physical, occupational, speech-language therapy, and assistive technologies—optimizes function and independence after acute illness, injury, or exacerbation of chronic disease. Effective rehab starts early, sets measurable goals (mobility, ADLs, communication), and coordinates with the medical plan. Globally, rehabilitation is recognized as essential to health systems, not optional, with WHO noting its role in reducing disability and improving participation in daily life. In practice, structured rehab prevents deconditioning, shortens recovery time, and helps people return to work or caregiving roles sooner.
Why it matters
- WHO: rehab is a set of interventions to optimize functioning and reduce disability; expanding access is a global priority.
How to do it
- Set SMART goals: e.g., “walk 300 meters with cane in 2 weeks.”
- Dose therapy: 20–45 minutes, 3–5 days/week (tailor to fatigue and safety).
- Measure: 6-minute walk test, grip strength, AM-PAC “6-Clicks.”
- Integrate home: assign daily micro-sessions (5–10 minutes) between visits.
Numbers & guardrails
- Falls risk protocols: home safety check within 72 hours; remove loose rugs; install grab bars if needed.
Bottom line: A coordinated rehab plan turns recovery from a vague hope into measurable progress toward independence.
7. Structured Care Transitions & Navigation
Transitions—from hospital to home, rehab, or primary care—are fragile moments where errors cluster. A structured discharge and navigation plan reduces medication problems, missed follow-ups, and avoidable readmissions. Programs that include medication reconciliation, clear “who to call” instructions, prompt follow-up, and caregiver education show lower readmissions and shorter stays in many settings. Assigning a navigator (nurse, pharmacist, social worker) to shepherd the first 30 days helps catch issues before they escalate.
Why it matters
- Patient- and family-centred transition interventions are linked with fewer readmissions; integrated care can reduce admissions and length of stay.
How to do it
- IDEAL discharge: Include, Discuss, Educate, Assess, and Listen.
- Book follow-ups before discharge: primary care/specialist within 7–14 days.
- Brown-bag review: pharmacist reconciles meds with the patient’s actual bottles.
- Two calls: 48-hour check-in and day-10 escalation sweep.
Mini case
- A community hospital’s daily integrated care conferences for COPD cut length of stay—showing how disciplined coordination pays off.
Bottom line: A named navigator and a repeatable discharge bundle tame the most error-prone phase of recovery.
8. Self-Management Education & Patient Activation
People recover faster when they understand their condition and believe they can influence it. Self-management programs (like the Stanford Chronic Disease Self-Management Program, CDSMP) teach skills for problem-solving, action planning, and shared decision-making. Evidence shows gains in self-efficacy, healthier behaviors, and quality of life, with some studies reporting reduced utilization. The Patient Activation Measure (PAM) offers a practical way to gauge a person’s knowledge, skills, and confidence; raising activation levels is associated with better outcomes and more efficient care.
Why it matters
- CDSMP meta-analyses report improvements in self-efficacy and health-related outcomes at 6 months.
- PAM is a validated tool to tailor education and track progress.
How to do it
- Offer a 6-week course: 2 hours/week group sessions or digital modules.
- Use micro-goals: “Walk 10 minutes after lunch daily” beats vague intentions.
- Measure activation: PAM at baseline and 12 weeks to tailor support.
- Close the loop: share a simple dashboard of goals, symptoms, and meds.
Mini-checklist
- Plain-language materials, bilingual options, large fonts, and pictograms for low literacy.
Bottom line: Education plus activation turns people into confident partners—improving adherence and day-to-day decision-making.
9. Social & Practical Supports (SDOH): Transport, Money, Work & Home
Recovery isn’t only about prescriptions; it hinges on transportation, income, housing, food, and safe home environments. The CDC defines these “social determinants of health” (SDOH) as nonmedical factors that shape outcomes. Transportation barriers alone lead to delayed care and missed medications, with disproportionate impact in rural areas and for people on lower incomes. Solutions include ride benefits, mobile services, employer flexibility, and home modifications—all of which keep treatment plans feasible. Build these supports into the care plan, not as afterthoughts.
Why it matters
- Transportation barriers are linked with missed appointments and poorer chronic disease control; more than 5.8 million U.S. adults delayed care for lack of transport in a recent estimate. PMC
How to do it
- Ask every time: “Do you have a way to get to your appointment?”
- Line up options: vouchers, paratransit, community drivers, telehealth substitution.
- Stabilize the home: food delivery during flares; temporary ramps or grab bars.
- Work/school: request formal accommodations and flexible scheduling.
Mini-checklist
- Screen SDOH on intake, document barriers, assign a CHW or social worker, and track closure of each need.
Bottom line: When social and practical needs are solved, adherence rises and recovery plans stick.
FAQs
1) What is the single most important support I should set up before discharge?
Name one caregiver or friend as your primary point of contact and include them in discharge teaching. Give them the one-page plan (med list, warning signs, who to call) and book follow-ups before you leave. Evidence shows patient- and family-centred transition processes are tied to fewer readmissions—especially in the first 30 days.
2) Do support systems really change hard outcomes like survival?
Yes. Social isolation is associated with higher all-cause mortality in meta-analyses, suggesting that strong relationships and integration into care matter beyond comfort and convenience. While causality can be complex, the association is consistent across populations and study designs.
3) I live far from the clinic—can telehealth replace in-person visits?
Often, telehealth can safely handle follow-ups, medication adjustments, and symptom checks, especially when paired with simple home devices (e.g., a blood pressure cuff). Patient satisfaction is high in many chronic disease programs, and virtual care reduces transportation barriers—but some exams and tests still require in-person visits.
4) How do I know if my education efforts are working?
Use the Patient Activation Measure (PAM) or similar tools. If activation rises by ~3 points or more over time, people generally show better self-management and engagement. Pair measurement with practical changes—short goals, teach-back, and easy-to-use materials. p4qm.org
5) What’s the difference between peer support and therapy?
Peer support offers experiential guidance and mutual accountability; therapy provides clinical assessment and treatment by licensed professionals. They can complement each other: peers sustain daily habits and motivation; clinicians adjust diagnoses and medications. Evidence finds peer programs improve self-efficacy and coping across conditions, but they do not replace medical or psychological care.
6) We don’t have many specialists in my area—what else helps?
Community Health Workers and social prescribing link workers can close gaps by coordinating services, troubleshooting barriers, and keeping you engaged between scarce clinic visits. Programs in diverse settings show improvements in screening, control of chronic conditions, and follow-up adherence.
7) How do I measure whether my support system is “working”?
Track a small set of outcomes for 30–90 days: medication adherence (>90% of doses), appointment attendance (>85%), symptom trend (e.g., days with dyspnea), and urgent care use (aim downward). Add a patient-reported outcome like pain or fatigue and a functional measure (e.g., 6-minute walk distance).
8) Does rehabilitation matter if I’m “only” dealing with a medical illness, not an injury?
Absolutely. Rehabilitation isn’t only for injuries; it helps optimize function and independence for people with chronic or complex medical conditions (e.g., COPD, heart failure, cancer). Early, goal-oriented rehab reduces disability and supports return to daily roles.
9) What if my family can’t help—how do I build a support system?
Start with your care team’s social worker to map local resources: CHWs, disease-specific groups, faith-based volunteers, transport services, and telehealth options. Ask for a navigator for the first month post-discharge and join a moderated peer community relevant to your condition.
10) Are there risks to caregiver involvement?
Caregivers can experience burnout, financial stress, and role strain. Build respite into the plan, share tasks, and teach caregivers to escalate early. Some studies show mixed effects when identification is formal but support is thin—engagement must come with training and resources. aging.jmir.org
Conclusion
Recovery accelerates when you treat support as part of the therapy, not a nice-to-have. The nine pillars above work together: caregivers translate instructions into daily routines; peers reinforce habits; multidisciplinary teams coordinate safe handoffs; CHWs and social prescribing remove practical barriers; telehealth keeps feedback loops tight; rehabilitation restores function; transitions and navigation prevent loose ends; self-management education lifts confidence; and social supports keep the whole plan feasible. Choose two or three pillars to strengthen this week—name a caregiver, schedule a telehealth follow-up, and request a CHW referral—then expand from there. Over 30–90 days, track simple metrics and adjust. A stronger support system is one of the most powerful, evidence-backed ways to improve outcomes and quality of life. Next step: share this article with your caregiver and care team, and pick your first three actions today.
References
- Social isolation as a risk factor for all-cause mortality: a systematic review and meta-analysis, PLOS ONE, 2023. https://pmc.ncbi.nlm.nih.gov/articles/PMC9836313/
- Guide to Patient and Family Engagement in Hospital Quality and Safety, Agency for Healthcare Research and Quality (AHRQ), updated 2023. https://www.ahrq.gov/patient-safety/patients-families/engagingfamilies/guide.html
- Strategy 4: Care Transitions From Hospital to Home—IDEAL Discharge Planning, AHRQ, updated 2023. https://www.ahrq.gov/patient-safety/patients-families/engagingfamilies/strategy4/index.html
- Patient- and family-centred care transition interventions for older adults: systematic review, BMC Geriatrics, 2023. https://pmc.ncbi.nlm.nih.gov/articles/PMC10750974/
- The impact of interdisciplinary team-based care on chronically ill patients: systematic review, Journal of Multidisciplinary Healthcare, 2025. https://pmc.ncbi.nlm.nih.gov/articles/PMC11789502/
- Teamwork and its impact on chronic disease clinical outcomes: review, Public Health, 2024. https://www.sciencedirect.com/science/article/pii/S0033350624000398
- Peer support for people with chronic conditions: a scoping review, Chronic Illness, 2022. https://pmc.ncbi.nlm.nih.gov/articles/PMC8973527/
- Community health workers bring value and deserve to be paid, Lancet Regional Health – Americas, 2023. https://pmc.ncbi.nlm.nih.gov/articles/PMC10030954/
- Evaluation of the effectiveness of telehealth chronic disease management, Healthcare (Basel), 2023. https://pmc.ncbi.nlm.nih.gov/articles/PMC10176143/
- Rehabilitation—Fact Sheet, World Health Organization, April 22, 2024. https://www.who.int/news-room/fact-sheets/detail/rehabilitation
- Impact of integrated care on patient-related outcomes: review, International Journal of Integrated Care, 2019. https://pmc.ncbi.nlm.nih.gov/articles/PMC6659761/
- The effectiveness of the Chronic Disease Self-Management Program: systematic review, International Journal of Environmental Research and Public Health, 2024. https://pmc.ncbi.nlm.nih.gov/articles/PMC11011545/
- Development of the Patient Activation Measure (PAM), Health Services Research, 2004. https://pmc.ncbi.nlm.nih.gov/articles/PMC1361049/
- Social Determinants of Health (SDOH): Why they matter, Centers for Disease Control and Prevention, Jan 17, 2024. https://www.cdc.gov/about/priorities/why-is-addressing-sdoh-important.html
- Transportation barriers to health care in the United States, American Journal of Public Health, 2020. https://pmc.ncbi.nlm.nih.gov/articles/PMC7204444/
- A systematic review of interventions to minimize transportation barriers to healthcare access, BMC Public Health, 2019. https://pmc.ncbi.nlm.nih.gov/articles/PMC6450539/
- Daily integrated care conferences to reduce length of stay in COPD exacerbations, Journal of the American Osteopathic Association, 2020. https://pubmed.ncbi.nlm.nih.gov/32091558/