A reliable bedtime routine turns late-night battles into predictable, peaceful evenings. In plain terms, a toddler bedtime routine is a short, repeated sequence of calming steps—done at the same time, in the same order—that helps your child fall asleep sooner and sleep more soundly. Done well, it aligns with how much sleep toddlers need (including naps), cues the body for rest, and gives caregivers a simple script to follow on hectic nights. This guide is for ages 1–3 and blends evidence-based sleep science with real-life tools. Quick start: choose a target bedtime, begin wind-down 30–40 minutes before, follow “Brush, Book, Bed,” keep the room dark and cool, cap late naps, and respond to night wakings with brief, consistent check-ins. This article is informational and not a substitute for medical advice—speak with your pediatrician for individualized guidance.
1. Lock Your 24-Hour Sleep Targets First (Then Fit the Routine Around Them)
Start by deciding how much total sleep your toddler needs and when it will happen; the routine will work only if the schedule works. Children 1–2 years typically need 11–14 hours of sleep across 24 hours, and children 3–5 years need 10–13 hours (including naps). That range gives you flexibility to balance one daytime nap with consolidated night sleep. Choose a consistent wake time (the true anchor of the schedule), then place bedtime 11–12 hours after wake time, subtracting nap length. This top-down planning prevents two common problems: bedtimes that drift later every week and overtired toddlers who fight sleep. It also makes weekday/weekend schedules similar enough that your toddler’s internal clock doesn’t reset on Mondays.
1.1 Why it matters
A predictable 24-hour rhythm helps toddlers fall asleep faster and stay asleep longer. Research-based sleep duration targets from sleep medicine organizations are tied to better behavior, learning, and health outcomes in early childhood. When you work backward from wake time, bedtime becomes a decision, not a debate.
1.2 How to do it
- Pick a wake time you can keep within ±30 minutes daily.
- Choose a single daytime nap of ~60–120 minutes (most 1–3-year-olds).
- Subtract nap length from the daily total to set night-sleep goals.
- Place bedtime so your toddler is in bed 20–30 minutes before the target “asleep” time.
- Keep wake time and nap start within consistent windows, even on weekends.
Numbers & guardrails: As of August 2025, expert consensus recommends 11–14 hours (1–2 years) and 10–13 hours (3–5 years) per 24 hours, inclusive of naps. If bedtime creeps later than planned more than three nights in a week, your schedule is too ambitious—shift the nap earlier or shorten it slightly.
Synthesis: Decide the total sleep, then schedule the day; your routine will “click” because it fits your toddler’s biology.
2. Start Wind-Down 30–40 Minutes Before Lights-Out
Your routine should be short, repeatable, and calm—long enough to cue sleep but not so long that everyone loses patience. A 30–40 minute wind-down reliably lowers arousal, slows the pace of the evening, and creates space for connection without stalling bedtime. Families often find that once they move bath, pajamas, toothbrushing, and stories into a tight sequence, protests drop because the “what’s next?” questions disappear. The routine also helps transition from bright living spaces and stimulating play to a dark, quiet bedroom where sleep feels natural.
2.1 Why it matters
Studies show that introducing a consistent bedtime routine in young children improves sleep onset and reduces night wakings, with benefits seen within days and sustained over weeks. Keeping the routine concise increases the odds you’ll actually stick to it on busy nights.
2.2 Mini-checklist
- Begin 30–40 minutes before target “lights-out.”
- Keep the same order nightly (e.g., bath → pajamas → brush → books → bed).
- Avoid adding “one more thing” at the door; end with a predictable phrase.
- If bath excites your toddler, move it earlier or skip it on some nights.
- Aim for the bedroom to be dim and quiet for the last 10–15 minutes.
Numbers & guardrails: Many pediatric sources suggest ~30 minutes for most kids, extending slightly if a bath is included. If your wind-down exceeds 45 minutes regularly, trim steps or start earlier. Evidence links consistent routines with faster sleep onset and better parent-reported sleep. ScienceDirect
Synthesis: A short, same-order ritual lowers resistance and gets your toddler from play mode to sleep mode—night after night.
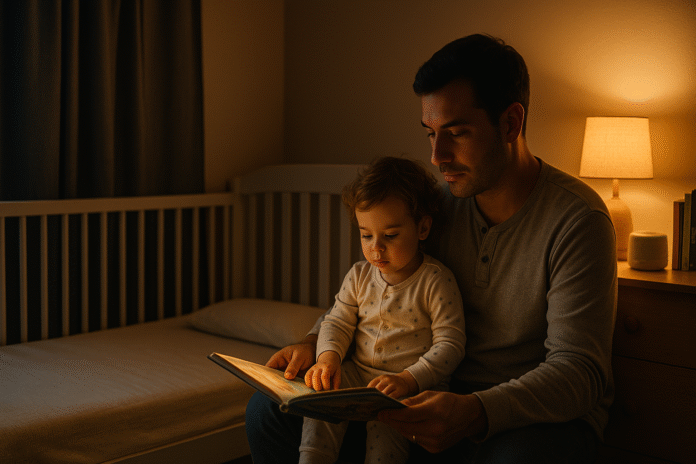
3. Use “Brush, Book, Bed” to Structure the Final 15–20 Minutes
A memorable sequence keeps everyone on track. “Brush, Book, Bed,” an American Academy of Pediatrics program, wraps oral health, literacy, and sleep cues into three simple steps: brush teeth, read a book (or two), and get to bed at a regular time. It’s toddler-friendly, creates positive attention where you want it, and helps end the day with connection. Crucially, brushing is placed before reading so the last thing on the teeth is fluoride toothpaste—helpful for cavity prevention.
3.1 How to do it
- Brush: Use a smear of fluoride toothpaste (grain of rice) until age 3, then a pea-sized amount; brush for ~2 minutes.
- Book: Read 1–3 calm stories; dim the light enough for you to see but low enough to cue “night.”
- Bed: Short good-night phrase, lights out, then into bed awake.
3.2 Common mistakes
- Giving milk or juice after brushing (raises cavity risk).
- Letting books become an open-ended negotiation (“just one more…”).
- Skipping brushing “because they’re tired” (it gets harder to restart).
Numbers & guardrails: The AAP’s Brush, Book, Bed program recommends this exact order nightly. Pediatric dental guidance supports brushing twice daily and making bedtime brushing non-negotiable. AAPD
Synthesis: Use a simple, memorable script—Brush, Book, Bed—to end on connection while protecting teeth and sleep.
4. Optimize the Sleep Environment: Dark, Cool, and Quiet (Enough)
Even the best routine struggles against a bright, noisy, or stuffy room. Toddlers sleep best in a dark bedroom (use blackout curtains and cover bright LEDs), a comfortably cool temperature, and a steady background sound that masks household noise if needed. While exact temperatures vary by home and climate, many families aim for roughly 18–22°C (64–72°F); baby-focused organizations cite 16–20°C as comfortable/safe for younger children, which remains a reasonable, conservative target for toddlers. If you use a sound machine, keep it across the room and at a low volume.
4.1 Tools & examples
- Blackout curtains; dimmable lamp for reading.
- A basic fan or quiet white-noise machine placed several feet from the bed.
- Room thermometer and breathable sleepwear to avoid overheating.
- Remove stimulating toys from the sleep space.
4.2 Numbers & guardrails
- Keep sleep spaces cool; UK/NHS and child-sleep charities cite 16–20°C as a safe baby room temperature (toddlers tolerate similar).
- For white noise, pediatric research recommends sound levels at or below ~50 dBA in nurseries; place devices away from the bed and use the lowest effective volume.
- Avoid loose cords and position devices out of reach. Lullaby Trust
Synthesis: A darker, cooler, quieter room increases your routine’s success without adding a single extra step.
5. Time Naps to Protect Bedtime (and Guard Against Overtiredness)
Naps are vital for toddlers—but when and how long they nap affects bedtime like a lever. Long or late afternoon naps can push sleep onset later and shorten night sleep; too little daytime sleep can backfire with an overtired toddler who melts down at bedtime. The sweet spot for many families is one midday nap of about 60–120 minutes, ending by mid- to late afternoon so that enough sleep pressure builds before bed.
5.1 Numbers & guardrails
- Total daily sleep needs (including naps): 11–14 hours (1–2 years) and 10–13 hours (3–5 years).
- Evidence links late or long naps to later sleep onset and shorter night sleep in toddlers.
- On days with unusually long/late naps, shift bedtime later by ~15–30 minutes to avoid battles.
5.2 Mini-checklist
- Protect the nap start time (±30 minutes) and nap length (set a quiet timer for wake-up).
- Avoid naps starting in the late afternoon unless you plan a later bedtime.
- If the nap is skipped, begin wind-down earlier and expect an earlier bedtime.
- Keep pre-nap and pre-bed routines similar (shorter for naps).
Synthesis: Treat nap timing as part of the bedtime routine; well-timed naps make bedtime easier, not harder.
6. Cut Evening Stimulation: Screens Off, Sugar Low, Lights Dim
Toddlers wind down best when the evening is calm. Bright screens and fast-paced content can delay sleep through stimulation and short-wavelength (blue) light effects on melatonin. The American Academy of Pediatrics recommends avoiding screens for at least one hour before bed and keeping devices out of bedrooms. Likewise, save sugary foods and caffeine (including chocolate) for earlier in the day. As you enter the wind-down window, dim household lighting and switch to warm, low-light lamps.
6.1 How to do it
- Set a household “screens off” rule 60–90 minutes before bedtime.
- Move energetic play earlier; switch to puzzles, coloring, or gentle music.
- Use warm lamps or dimmers after dinner; turn overhead lights off.
- Offer water after brushing—but avoid milk/juice to protect teeth.
6.2 Numbers & guardrails
- As of August 2025, AAP guidance advises avoiding screens for at least 1 hour before bedtime and keeping phones out of bedrooms.
- Blue-light effects are real, but stimulation/content also matters; keep evenings calm. American Academy of Pediatrics
Synthesis: Quiet, low-light evenings help your routine work as intended—no battles with bright screens or sugary second winds.
7. Add Predictable Choices and Comfort Objects (After 12 Months)
Routines stick when toddlers feel some control. Offer small, pre-approved choices—“blue or green pajamas?” “this book or that one?”—to reduce power struggles. A consistent comfort object (lovey) can also ease separation at lights-out. Soft items carry suffocation risk in infancy, but after 12 months most experts consider a small blanket or lovey low risk for healthy children; many families wait until age 2 to introduce pillows. Keep items simple and limit volume—your toddler doesn’t need a menagerie in bed.
7.1 Tools & examples
- Two pajama options, two book options, one stuffed animal.
- A short “good-night” script you repeat nightly.
- Place a favorite photo by the bed if separation is tough.
7.2 Numbers & guardrails
- Keep soft objects out of infant sleep spaces; risk drops after 12 months.
- Consider waiting until ~2 years for a toddler pillow; choose small and firm.
- Limit “just one more” by offering choices earlier in the routine.
Synthesis: Boundaried choices + a simple comfort item calm protests without derailing safety or structure.
8. Teach Independent Sleep Onset with Gentle, Evidence-Based Methods
Falling asleep independently is a skill. Graduated check-ins (“Ferber”/modified extinction), bedtime fading, and the Bedtime Pass are well-studied approaches that improve bedtime resistance and reduce night wakings without long-term harm to attachment or behavior. Choose the least-disruptive method that fits your family values; pair it with a consistent routine for best results.
8.1 Options that work
- Graduated check-ins: Put your toddler down awake; return briefly at set or increasing intervals if they protest.
- Bedtime fading: Temporarily delay bedtime to the time your toddler naturally falls asleep, then move it earlier by ~10–15 minutes every few nights.
- Bedtime Pass (for “door-dashing” preschoolers): Give one “pass” for a quick extra request; after it’s used, returns are calmly ignored until morning.
8.2 Numbers & guardrails
- Randomized and clinical trials show that consistent routines, graduated checks, bedtime fading, and the Bedtime Pass improve sleep in young children; benefits can appear within days.
- Keep check-ins brief (15–60 seconds), neutral, and consistent; expect resistance to peak then drop (an “extinction burst”).
- If distress escalates beyond what you’re comfortable with, pause and try a gentler approach.
Synthesis: A predictable routine plus a structured response plan teaches self-settling in a way that fits your family.
9. Plan for Night Wakings and Early Rising (Before They Happen)
Even great sleepers wake at night; your plan determines whether they resettle or fully wake. Keep responses brief, boring, and consistent: a short check at the door, a quiet phrase, a tuck-in, then leave. For early risers, push morning light exposure later (keep the room dark until the allowed time) and use an “OK-to-wake” clock so your toddler learns the green light means morning. If night wakings come with snoring, gasping, or persistently restless sleep, talk with your pediatrician about screening for obstructive sleep apnea.
9.1 Mini-checklist
- Treat wake-ups consistently; avoid starting new props at 2 a.m.
- Keep the room dark overnight; delay morning light until “wake” time.
- Use a simple visual clock for 2.5–3-year-olds and up.
- Consider capping late naps that push bedtime too far.
9.2 Numbers & guardrails
- Loud, persistent snoring, gasping, or witnessed pauses in breathing are red flags for sleep apnea—seek medical advice.
- Daytime outcomes (mood, attention) are as important as night metrics when evaluating progress.
Synthesis: Decide your night-response rules in daylight; consistency at 2 a.m. is the fastest path back to sleep.
10. Keep Routines on Track Through Travel, Illness, and Clock Changes
Life happens—routines get bumped by travel, teething, and Daylight Saving Time. Rather than starting from scratch, preserve the routine’s order and feel wherever you are. Pack a “sleep kit” (favorite PJs, books, compact blackouts, white-noise app) and re-create the bedroom cues. For clock changes, shift schedule and routine earlier or later in 10–15 minute increments over several days. During illness, prioritize comfort and safety, then return to normal as soon as your child feels better—consistency rebounds quickly if you keep the routine recognizable.
10.1 Tools & examples
- Travel blackout shades or painter’s tape + trash bags in a pinch.
- A small tote with toothbrush, two favorite books, lovey, and a nightlight.
- For spring DST, nudge bedtime and wake time 10–15 minutes earlier for 3–4 days.
10.2 Numbers & guardrails
- Pediatric organizations suggest gradual schedule shifts around daylight changes; avoid abrupt one-hour jumps if your toddler is sensitive.
- Keep screens off before bed even when routines are disrupted; use books as the reliable anchor.
Synthesis: When life shifts, keep the routine’s bones intact—order, tone, and environment—so your toddler’s sleep gets back on track fast.
FAQs
1) What time should my toddler go to bed?
Work backward from wake time using age-based totals: 11–14 hours (1–2 years) and 10–13 hours (3–5 years), including naps. If your toddler wakes at 7:00 a.m. and naps 1.5 hours, aim for ~10.5–11.5 hours of night sleep—bedtime around 7:30–8:00 p.m. Keep a consistent wake time within ±30 minutes to stabilize bedtime. PMC
2) How long should the bedtime routine take?
Most families do well with 30–40 minutes. Longer routines often become negotiation arenas; shorter routines can feel rushed. If you include a bath, start earlier or move the bath earlier in the evening on busy nights. Sleep Foundation
3) Do I really need to turn off screens?
Yes—especially in the hour before bed. The AAP recommends avoiding screens for at least 1 hour pre-bed and keeping devices out of bedrooms. Blue light and stimulating content both interfere with winding down. Replace screens with quiet play or books.
4) What about white-noise machines—are they safe?
Used correctly, yes. Keep the device across the room and at the lowest effective volume; research suggests nursery sound levels at or below ~50 dBA. Don’t place devices in or on the bed, and keep cords out of reach.
5) Is it okay to give milk right before bed?
Offer milk earlier in the evening. After brushing, stick to water only to protect teeth. Place toothbrushing within your routine (Brush, Book, Bed), so the toothbrush is the last thing to touch teeth before lights-out.
6) When can my toddler have a pillow or blanket?
Soft items should be kept out of infant sleep spaces. After 12 months, risk drops for healthy children; many families wait until around age 2 to introduce a small, firm pillow. Keep bedding minimal and ensure your child can move it away from their face. HealthyChildren.orgAAP Publications
7) Why is my toddler wide awake after a long nap?
Late or long naps reduce sleep pressure, pushing bedtime later and shortening night sleep. Aim to end naps by mid- to late afternoon and consider trimming unusually long naps by 15–30 minutes if bedtime stalls.
8) Which sleep-training method is “best” for toddlers?
The best method is one you can do consistently. Evidence supports several approaches—graduated check-ins, bedtime fading, and the Bedtime Pass—to reduce bedtime resistance and night wakings. Start gently and adjust if distress feels too high. PMCPubMed
9) My child snores—is that normal?
Occasional snoring with a cold is common. Persistent, loud snoring; gasping; or pauses in breathing warrant a pediatric evaluation for obstructive sleep apnea. Early treatment improves sleep quality and daytime behavior.
10) How do we handle travel or Daylight Saving Time?
Preserve the routine’s order and vibe; pack key cues (books, PJs, portable blackouts, white noise). Shift sleep times by 10–15 minutes over several days before clock changes. Expect a short adjustment period—consistency brings sleep back in line.
Conclusion
A consistent toddler bedtime routine isn’t magic—it’s a smart sequence that lines up with your child’s biology and your family’s life. Start by locking your 24-hour sleep targets and protecting nap timing so bedtime has a fighting chance. Keep wind-down short and repeatable; anchor the final minutes with Brush, Book, Bed; and optimize the bedroom for darkness, coolness, and quiet. Then, layer in predictable choices, keep evenings low on stimulation, and pick a gentle, evidence-based plan for teaching independent sleep. Night wakings, travel, and colds will happen; your job is to preserve the routine’s order and feel so your toddler’s body keeps recognizing “it’s time to sleep.” If you stay consistent with the plan above for 10–14 nights, you’ll typically see faster bedtimes, fewer wake-ups, and calmer evenings. Ready to begin? Choose a wake time, pick tonight’s 30-minute wind-down, and print a simple “Brush, Book, Bed” card for the bathroom mirror.
CTA: Post tonight’s routine on the fridge, set a “screens-off” alarm, and start your 30-minute wind-down this evening.
References
- Consensus Statement of the American Academy of Sleep Medicine on the Recommended Amount of Sleep for Pediatric Populations, AASM (Paruthi et al.), 2016. https://pmc.ncbi.nlm.nih.gov/articles/PMC5078711/
- Recommended Amount of Sleep for Pediatric Populations (PDF), AASM, 2016. https://aasm.org/resources/pdf/pediatricsleepdurationconsensus.pdf
- Child Sleep Duration Health Advisory, American Academy of Sleep Medicine, Sept 13, 2019. https://aasm.org/advocacy/position-statements/child-sleep-duration-health-advisory/
- Benefits of a bedtime routine in young children: Sleep, development and wellbeing, Sleep Medicine Reviews (Mindell et al.), 2018. https://pmc.ncbi.nlm.nih.gov/articles/PMC6587181/
- Implementation of a nightly bedtime routine: How quickly do things improve?, Sleep Medicine (Mindell et al.), 2017. https://pmc.ncbi.nlm.nih.gov/articles/PMC6587179/
- Brush, Book, Bed: How to Structure Your Child’s Nighttime Routine, HealthyChildren.org (AAP), updated 2023. https://www.healthychildren.org/English/healthy-living/oral-health/Pages/Brush-Book-Bed.aspx
- Good Oral Health Starts Early: Brushing Up on Oral Health—Never Too Early to Start, HealthyChildren.org (AAP), Dec 19, 2022. https://www.healthychildren.org/English/healthy-living/oral-health/Pages/Brushing-Up-on-Oral-Health-Never-Too-Early-to-Start.aspx
- Melatonin for Kids: What Parents Should Know About This Natural Sleep Aid, HealthyChildren.org (AAP), Apr 27, 2023 — section on screens and sleep. https://www.healthychildren.org/English/healthy-living/sleep/Pages/melatonin-and-childrens-sleep.aspx
- Infant Sleep Machines and Hazardous Sound Pressure Levels, Pediatrics (Hugh et al.), 2014. https://publications.aap.org/pediatrics/article/133/4/677/32749/Infant-Sleep-Machines-and-Hazardous-Sound-Pressure
- How to dress a newborn baby – Safe room temperature, NHS Start for Life, 2023. https://www.nhs.uk/start-for-life/baby/baby-basics/caring-for-your-baby/how-to-dress-a-newborn/
- Daytime nap controls toddlers’ nighttime sleep, Sleep and Biological Rhythms (Nakagawa et al.), 2016. https://pmc.ncbi.nlm.nih.gov/articles/PMC4899693/
- Obstructive Sleep Apnea—Signs and Symptoms, Children’s Hospital of Philadelphia, accessed 2025. https://www.chop.edu/conditions-diseases/obstructive-sleep-apnea
- Daylight Saving Time: Don’t Lose Sleep Over It, HealthyChildren.org (AAP), Oct 30, 2024. https://www.healthychildren.org/English/healthy-living/sleep/Pages/daylight-saving-time-dont-lose-sleep-over-it.aspx
- Healthy Sleep Habits (sleep tips by age), Children’s Hospital of Philadelphia, accessed 2025. https://www.chop.edu/primary-care/healthy-sleep-habits