Support-seeking isn’t just a personal choice—it’s shaped by identity, family, faith, language, and local systems. This guide explains how culture influences when, where, and how people seek help, and it offers practical ways to engage care that’s both effective and respectful. It’s written for anyone navigating care across cultures: individuals, families, clinicians, educators, and community leaders. In brief: “Cultural perspectives on seeking support” means the beliefs, norms, and structures that shape whether people turn to family, faith leaders, traditional healers, or professionals—and what “good help” looks like in their context. As a quick start, map preferences, decision-makers, support types, and privacy needs before choosing a pathway. (Educational content only; not a substitute for medical advice.)
Quick start steps: identify the person’s preferred helpers (family/faith/professional), ask what “getting better” means to them, clarify privacy expectations, match modalities (e.g., peer group, therapist, traditional healer), and agree on concrete next steps.
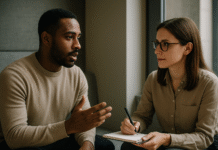
1. Center Cultural Explanatory Models (Not Just Diagnoses)
Start by asking people how they understand the problem and what improvement would look like; this clarifies whether support should begin with family, faith, traditional healers, or clinical care. The fastest way to do this respectfully is to explore their explanatory model—their own story for what’s happening, why now, and what helps. This approach prevents mismatch (for example, offering medication when a person first expects family mediation or pastoral support) and builds trust early. Tools like Arthur Kleinman’s questions and the DSM-5 Cultural Formulation Interview (CFI) provide structured prompts for any setting. They don’t replace diagnosis; they make care usable by aligning with lived meaning, values, and help-seeking norms. These tools are widely used across specialties to surface beliefs, social stressors, spiritual frames, and barriers to care.
1.1 Why it matters
- Fit before fix: When help matches the person’s model, engagement and follow-through rise.
- Trust builder: Asking “what do you call this problem?” signals respect for local knowledge.
- Stigma buffer: Normalizes talking about distress using familiar language.
- Navigation aid: Reveals preferred entry points (e.g., family elder, imam, GP, traditional healer).
1.2 How to do it
- Use the CFI’s short prompts (e.g., “What do you think is causing this?”).
- Ask what outcomes matter (sleep? family peace? daily function?).
- Map “help firsts” (home remedies, rituals, counseling, medication).
- Close by agreeing on a blended plan (e.g., counseling + family meeting).
Mini-case: A student describes “nerves” and family conflict, not “anxiety.” After a short CFI-style conversation, the plan includes a family check-in, a school counselor referral, and permission to involve a youth pastor—improving buy-in from the start.
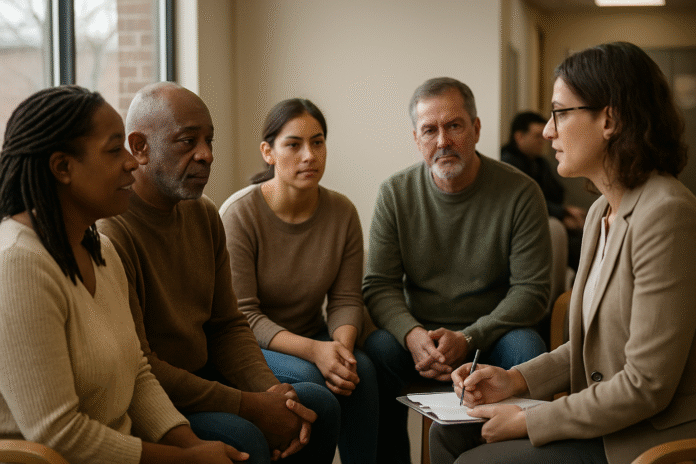
2. Respect Collectivism and Individualism (Who Decides—and With Whom)
Whether people seek help privately or with family is deeply cultural. In collectivist contexts, decisions often involve parents, spouses, or elders; in individualist settings, autonomy and confidentiality lead. A respectful plan clarifies who has a say, who attends sessions, and when family involvement helps or harms. In Latinx families, familismo can be a powerful support—mobilizing care, transportation, and adherence—but it can also delay professional help if problems are kept “within the family.” Similarly, immigrants may prefer family or community leaders before clinics, especially where trust in institutions is low. The goal isn’t to label one approach “better,” but to align with values while preserving the person’s safety and rights.
2.1 Practical guardrails
- Ask, “Who do you want involved in decisions?”
- Offer options: joint sessions, elder briefings, or private 1:1 time.
- Name confidentiality boundaries plainly and early.
- If family delays care, negotiate small first steps (screening, psychoeducation).
2.2 Region-specific notes
- In many Middle Eastern and South Asian families, elder endorsement speeds help-seeking.
- For diaspora youth balancing cultures, dual-track plans (family + private support) often work best.
- In some contexts, public disclosure risks social stigma; plan discreet access points.
Bottom line: Clarify the decision-making circle—then design support that honors it without compromising safety.
3. Name Stigma and Language—Including Idioms of Distress
Stigma and language shape whether people seek help at all. Many cultures express distress somatically (“chest tightness,” “head pressure,” “weak blood”) or through cultural concepts of distress like ataque de nervios or khyâl (“wind”) attacks. Recognizing and translating these idioms into actionable care avoids dismissal and builds credibility. Using the person’s terms first, then connecting them to options (breathing, ritual, counseling, medication) reduces shame and medical mistrust. Evidence shows that stigma is widespread across cultures and that culturally relevant language improves engagement and outcomes.
3.1 Tools/Examples
- Language bridge: Mirror the person’s words (“wind rise,” “nerves”) before adding clinical terms.
- Education, not correction: Link idioms to body stress systems and practical strategies.
- Examples: Ataque de nervios (Caribbean/Latinx); khyâl attacks (Cambodian). Frontiers
3.2 Mini checklist
- Identify the idiom used, map triggers, offer matched coping (e.g., grounding, ritual + CBT).
- Validate somatic symptoms; rule out medical issues; offer stepped care options.
- Provide translated handouts that reflect local terms and remedies.
Takeaway: Speak the person’s language—literally and culturally—before you speak the clinic’s.
4. Engage Faith and Spiritual Leaders as Gateways (With Clear Roles)
In many communities, the first helpers are clergy—imams, pastors, priests, monks—who provide meaning, comfort, and triage. Partnering with faith leaders can reduce stigma, surface safety issues sooner, and smooth referrals, especially where mental health systems are under-resourced. Collaboration works best with clear boundaries: clergy provide spiritual care and social support; clinicians provide clinical assessment and treatment; both communicate (with consent) to align goals. Studies across Muslim, Christian, and other communities show that faith leaders are pivotal connectors when supported with training and referral pathways. Quod LibetPMC
4.1 How to collaborate
- Co-create referral scripts and crisis plans; offer mental-health first aid training.
- Invite clergy to psychoeducation sessions (consent-based).
- Provide fast, discreet referral routes for clergy—text line, named clinician.
- Share de-identified trends to guide sermons/workshops on stigma.
4.2 Common pitfalls
- Blurring roles (clergy asked to “treat” psychosis).
- Over-spiritualizing medical crises.
- Clinicians dismissing spiritual meaning that sustains hope.
Synthesis: Faith partnerships widen the front door to care—when roles and privacy are honored.
5. Value Traditional and Indigenous Healing—Integrate, Don’t Erase
Traditional remedies and healers (e.g., herbalists, curanderos, shamans, community elders) are trusted sources of help and meaning. Rather than positioning biomedical care against these practices, respectful plans blend them when safe: ritual + therapy; herbal teas + sleep hygiene; healer visits + medication supervision. Recognizing cultural syndromes (e.g., ataque de nervios, khyâl attacks) and community meaning reduces dropout and can improve adherence to evidence-based care. Clinicians should routinely ask about remedies and healers—and check for interactions or delays in urgent conditions. Global frameworks (WHO’s mhGAP) support context-fitting care and task-sharing beyond specialist clinics. PMC
5.1 Mini-checklist
- Ask what traditional supports help and how they’re used.
- Discuss safety (e.g., herb–drug interactions, fasting during medication).
- Invite healers (with consent) to align goals and warning signs.
- Offer “both-and” plans to preserve trust and medical safety.
Bottom line: Respectful integration retains culture as an asset while protecting against harm.
6. Address Gender Norms—Especially Masculinity and Shame
Across many cultures, men are less likely to seek professional help due to norms valorizing toughness, self-reliance, and emotional control. These norms can delay care until crises (addiction, violence, self-harm). Research links conformity to traditional masculine norms with lower help-seeking and poorer mental health, particularly for depression. Practical workarounds include male-friendly entry points (coaching, peer groups), brief and goal-focused sessions, and confidential digital options. Women and gender-diverse people face their own barriers—caregiving burdens, safety, and stigma—which need tailored solutions. Naming norms explicitly and offering dignifying alternatives increases uptake. American Psychological Association
6.1 How to make care approachable
- Offer evening hours and discreet booking (“well-being consult”).
- Emphasize performance outcomes (sleep, focus, work, parenting).
- Use brief screeners (PHQ-9/GAD-7) and shared metrics to track wins.
- Normalize “coach + clinician” models for practical goals.
6.2 Mini example
A men’s group frames therapy as “stress performance tune-ups,” pairs sessions with gym time, and reports higher retention without diluting clinical rigor.
Synthesis: Call out the norm, then design help that preserves dignity and privacy.
7. Plan for Migration, Acculturation, and Diaspora Realities
Immigrants and refugees often face a double bind: new systems in unfamiliar languages and enduring obligations to family and culture. Structural barriers (documentation fears, insurance, transport, work hours) combine with cultural ones (stigma, preference for informal supports). Reviews show that immigrants’ help-seeking is strongly shaped by family dynamics, perceived discrimination, and knowledge of services; solutions include trusted community health workers, multilingual navigation, and flexible appointment formats. In many diasporas, youth prefer private or digital help while elders prefer family- or faith-based support—dual-track plans keep both engaged.
7.1 Region-specific notes
- Middle Eastern contexts: family endorsement and religious framing can reduce stigma.
- South Asian diasporas: intergenerational expectations can delay care for girls/young women; discreet access helps.
- Latinx communities: familismo can both support and gatekeep access—plan accordingly. ScienceDirect
7.2 Action list
- Provide bilingual intake and translated materials.
- Map transport/childcare barriers; offer telehealth when safe.
- Use community navigators to bridge trust and logistics.
Key point: Pair cultural fit with logistics; both predict whether care actually happens.
8. Use Culturally Adapted, Evidence-Based Interventions (Not Generic Scripts)
Evidence supports culturally adapted versions of proven therapies (e.g., CBT) for diverse communities, including adaptations to language, values, metaphors, and family roles. Meta-analyses show that adapted CBT is effective for ethnic minority groups and can improve trust and acceptability. The adaptation process should be explicit (not improvisational): identify cultural targets (e.g., fatalism, honor, spirituality), co-design metaphors and examples, and test with users. Community health workers and peer specialists can deliver adapted interventions effectively when trained and supervised—especially in low-resource settings or where mistrust of institutions is high. PMC
8.1 Numbers & guardrails
- As of 2023–2024, reviews indicate adapted CBT yields clinically meaningful gains; some studies show parity with standard CBT in majority groups.
- Ensure fidelity: adaptations should add cultural resonance without losing core mechanisms (exposure, cognitive skills, behavioral activation). Wiley Online Library
8.2 Tools/Examples
- Swap idioms and metaphors (e.g., “balance wind” + paced breathing).
- Include family sessions where values emphasize collective harmony.
- Use spiritual coping where desired (prayer, gratitude rituals).
Takeaway: Evidence-based and culture-fit is not a trade-off—it’s the recipe for results.
9. Design for Privacy, Confidentiality, and “Face”
Many communities weigh help-seeking against risks to reputation, marriage prospects, employment, or family honor. Clarify what is documented, who can see it, and how information flows across schools, clinics, and insurers. Offer discreet access points (neutral clinic names, private entrances, telehealth), and set explicit boundaries for shared information when families are involved. In high-context cultures, protecting “face” can be decisive; solutions that minimize exposure—short visits, off-site labs, cash-pay screening—can unlock care without stigma. Global guidance stresses shifting routine mental health support into primary care and communities, which often lowers visibility and improves reach.
9.1 Mini-checklist
- Explain privacy laws in plain language; confirm understanding.
- Offer consent forms that let people choose who is included.
- Provide discreet scheduling and nondescript visit reasons.
- Use primary care integration where possible (less stigma).
Synthesis: Safety and dignity are clinical interventions—treat them as such.
10. Track Outcomes with Shared, Translated Metrics
Measurement builds trust when it’s collaborative and culturally tuned. Use brief, translated screeners (e.g., PHQ-9, GAD-7) alongside person-defined outcomes (“argue less with my brother,” “pray without panic,” “sleep 7 hours”). Explain that scores guide adjustments—not labels. At the system level, global burden data show huge, persistent gaps in care and financing, so local programs should transparently track engagement, symptom change, and function by subgroup to prove value and secure funding. Sharing small, visual gains often keeps families onboard.
10.1 Practical metrics
- Symptom scales each visit; weekly function goals; monthly family satisfaction.
- Dropout and no-show rates (by language/age/gender) to spot inequities.
- Community feedback loops (faith leaders, schools) for continuous improvement.
Bottom line: Measuring what matters to people—and showing change—sustains trust and funding. PMC
11. Navigate Systems Honestly: Cost, Access, and Task-Sharing
Culture shapes preferences, but systems determine feasibility. Globally, public spending on mental health hovers near ~2% of health budgets, and in many countries most funds still flow to inpatient institutions, not community care—leaving people to rely on family, faith, or informal helpers. That reality makes task-sharing crucial: training non-specialists and community workers to deliver proven interventions under supervision. Effective programs blend cultural trust with clinical oversight, extend hours, cut travel, and reduce stigma by embedding care where people already are. When resources are scarce, honesty about cost, waitlists, and alternatives allows families to choose pathways that work now, not someday.
11.1 What to ask locally
- Which services are free or low-cost? Where are the shortest waits?
- Are community health workers or peer groups available in your area?
- Can primary care deliver first-line care (per WHO mhGAP) while you wait?
11.2 Mini example
A city clinic partners with a mosque and a youth center to offer mhGAP-aligned brief counseling by trained lay providers, supervised weekly by a psychologist. Attendance doubles; average wait drops from 6 weeks to 10 days.
Synthesis: Culture-fit plus system-savvy—especially task-sharing—turns values into access. Frontiers
FAQs
1) What does “Cultural Perspectives on Seeking Support” actually mean?
It refers to the beliefs, norms, and structures that guide when people ask for help, who they ask (family, faith, healers, professionals), and what “good help” looks like. Frameworks like the DSM-5 Cultural Formulation Interview and Kleinman’s questions help surface these preferences so care starts in the right place and language. Palliative Care Network of Wisconsin
2) Is it safe to combine traditional healing with therapy or medication?
Often, yes—if you review practices for safety and interactions, agree on goals, and coordinate with all helpers (with consent). Research on cultural syndromes shows that integrating meaning-rich practices with evidence-based care can reduce dropout and improve trust. Check urgent red flags (e.g., psychosis, suicidality) where medical care shouldn’t be delayed. NCBI
3) How can families help without taking over?
Clarify roles up front: who attends sessions, what gets shared, and where privacy is essential. In collectivist settings, family endorsement can speed care, but it can also delay professional help. A blended approach—family meetings plus confidential 1:1 time—preserves dignity and momentum.
4) What if a person refuses help because of stigma?
Meet their language first (e.g., “stress,” “nerves,” “wind”) and offer discreet options (primary-care visits, telehealth). Short trials with concrete goals can build confidence. Evidence across cultures shows stigma is pervasive, so normalize help as a strength and a family investment in well-being.
5) Do men really avoid help more than women? Why?
Across cultures, conformity to traditional masculine norms—toughness, invulnerability, self-reliance—is associated with lower help-seeking and worse mental health, especially for depression. Practical fixes include male-friendly framing, brief outcomes-focused visits, and private access. ScienceDirect
6) What’s the evidence that cultural adaptations of therapy work?
Meta-analyses and reviews show adapted CBT is effective and can increase trust and acceptability in ethnic minority and global contexts, provided core mechanisms are preserved while language, metaphors, and values are tailored. PubMed
7) For immigrants and refugees, what helps most?
Trusted navigators (community health workers), multilingual materials, flexible scheduling, and family-sensitive planning improve uptake. Reviews of immigrant help-seeking highlight structural barriers and the importance of community connectors to bridge trust and logistics.
8) Are faith leaders part of the mental health system?
In many communities they’re the front door to support. Partnerships work best when roles are clear: spiritual care and social support from clergy, clinical care from clinicians, and warm referrals between them. Training and consent-based communication make the network safe and effective. HHS.gov
9) How do we protect privacy in close-knit communities?
Explain confidentiality plainly, document consent choices, and offer discreet access (primary care integration, neutral visit reasons, telehealth). Protecting “face” and reputation is often decisive for engagement. World Health Organization
10) Why do systems matter if culture is the focus here?
Because values can’t overcome closed doors. Globally, mental health receives around 2% of health budgets, often concentrated in hospitals, not community services. Task-sharing and primary-care integration (per WHO mhGAP) are practical ways to expand access now. The Lancet
Conclusion
Culture isn’t a barrier to care—it’s the context that makes care meaningful. When we begin with explanatory models, align with family and faith where desired, speak in local idioms, and protect privacy, help becomes both respectful and effective. Evidence shows that culturally adapted interventions work, and that partnerships with community and faith leaders widen the front door to care. Systems still matter: in many places, under-financing and long waits make task-sharing and primary-care integration essential bridges. Your next steps are straightforward: ask the person’s story of the problem, map decision-makers and privacy needs, co-choose a first helper, and track outcomes that matter at home. Do this, and you’ll convert good intentions into real access, adherence, and healing.
Call to action: Choose one principle above, apply it in your next conversation, and notice how trust—and help—moves forward.
References
- Mental Health Gap Action Programme (mhGAP) guideline for mental, neurological and substance use disorders. World Health Organization, 2023. IRIS
- Mental Health ATLAS 2020. World Health Organization, 2021. IRIS
- Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990–2019. The Lancet Psychiatry, 2022. https://www.thelancet.com/journals/lanpsy/article/PIIS2215-0366(21)00395-3/fulltext The Lancet
- Financing of Mental Health: A Global Imperative. United for Global Mental Health, 2023. United for Global Mental Health
- Cultural Formulation Interview (CFI). American Psychiatric Association (DSM-5 Tool), 2013. American Psychiatric Association
- Jarvis GE. Update on the Cultural Formulation Interview. Transcultural Psychiatry, 2020. PMC
- Ahad AA et al. Understanding and Addressing Mental Health Stigma Across Cultures: A Scoping Review. Frontiers in Psychiatry, 2023. PMC
- Sharan P. Cultural Issues Related to ICD-11 Mental, Behavioural and Neurodevelopmental Disorders. Indian Journal of Social Psychiatry, 2021. PMC
- Hinton DE et al. Khyâl Attacks: A Key Idiom of Distress Among Traumatized Cambodian Refugees. Journal of Anxiety Disorders, 2010. PubMed
- Villatoro AP et al. Family Culture in Mental Health Help-Seeking and Utilization in U.S. Latinos: A Systematic Review. Clinical Psychology Review, 2014. PMC
- Elshamy F et al. Mental Illness and Help-Seeking Behaviours Among Middle Eastern Populations: A Systematic Review. PLOS ONE, 2023. PLOS Journals
- Huey SJ Jr., Polo AJ. Culturally Responsive Cognitive Behavioral Therapy for Ethnic Minority Youth: A Review. Annual Review of Clinical Psychology, 2023. Annual Reviews
- Mohammadifirouzeh M et al. Factors Associated with Professional Mental Help-Seeking Among Immigrants in the U.S.: A Systematic Review. International Journal of Environmental Research and Public Health, 2023. PMC
- Rice S et al. Gender Norms and the Mental Health of Boys and Young Men. The Lancet Public Health, 2021. https://www.thelancet.com/journals/lanpub/article/PIIS2468-2667(21)00138-9/fulltext The Lancet
- Keynejad R et al. WHO Mental Health Gap Action Programme (mhGAP): Lessons and Next Steps. BJPsych International, 2021. PMC