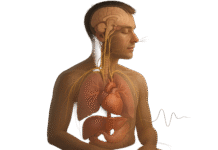
When stress spikes, your breath is the fastest lever you can pull. Diaphragmatic breathing—drawing air low so the belly and lower ribs expand—slows your rate, lengthens the exhale, and nudges the body’s relaxation response. In practice, that means steadier heart rhythms, a calmer mind, and a feeling of groundedness you can access anywhere. This guide teaches you exactly how to do it, from first setup to daily routines. You’ll learn safe pacing, common mistakes to avoid, and ways to use the technique during work, exercise recovery, and bedtime. This is educational information, not medical advice; if you have a respiratory or cardiac condition (e.g., COPD, asthma, arrhythmias), are pregnant, or feel dizzy when practicing, consult a clinician before proceeding.
Quick start (30–60 seconds): Sit tall or lie down. Place one hand on your chest and one on your belly. Inhale quietly through your nose so your belly and low ribs widen slightly; exhale through relaxed lips a bit longer than you inhale. Keep shoulders soft. Repeat 6–10 breaths.
1. Set Your Posture and Locate the Diaphragm
Good diaphragmatic breathing starts with a stable, open posture that lets the diaphragm descend and the lower ribs expand. Sit with your sit bones anchored, chest relaxed (not lifted), and the back of your neck long—as if a string draws the crown of your head upward. If you’re lying down, bend your knees and rest your feet flat to reduce low-back tension. The goal is simple: create space below the ribs so you can feel the belly gently move forward and the lower ribs widen on each inhale. If your shoulders creep upward or your low back arches hard, you’re compensating with accessory muscles instead of the diaphragm. Start where gravity helps—on your back or reclined—then progress to seated and standing as control improves.
1.1 How to do it
- Sit on the front third of a chair; feet flat, hips and knees at ~90°.
- Stack ears-over-shoulders-over-hips; imagine “soft chest, long spine.”
- Unlock the ribs: wrap hands around your lower ribcage to feel expansion.
- Keep jaw and tongue relaxed (tongue lightly on the roof of the mouth).
1.2 Numbers & guardrails
- Practice 2–5 minutes, 2–4 times per day at first.
- Keep effort low (2–3/10). If you’re straining, you’re doing too much.
- If you feel lightheaded, pause, return to normal breathing, and try fewer/shorter breaths next time.
Synthesis: A neutral, lengthened posture frees your diaphragm and sets every other step up for success; start low-effort so the pattern feels smooth and sustainable.
2. Use Hand Placement for Instant Feedback
The simplest way to know you’re doing it right is tactile feedback. Place one hand on your upper chest and one on your belly. On each inhale, the belly hand should move first and slightly more than the chest hand; on each exhale, both hands soften as air leaves. This immediate biofeedback teaches your body the pattern faster than thinking about “doing it right.” If your top hand lifts noticeably, you’re recruiting neck and chest muscles; if your belly hand barely moves, you’re probably holding your abdomen tight. Hand placement reduces overthinking and gives a yes/no signal you can check anytime—at your desk, on the couch, or in bed.
2.1 Mini-checklist
- Inhale: belly hand rises first → lower ribs widen → chest hand barely moves.
- Exhale: both hands fall; belly hand returns toward neutral.
- Noise: breath is quiet; no shoulder shrugging or neck tension.
2.2 Common mistakes
- Bracing the abs so the belly can’t move (loosen your belt/waistband).
- Forcing large breaths (go for small, smooth waves instead of big gulps).
- Rushing—aim for slower, longer, softer breaths.
Synthesis: Your hands turn an invisible skill into a visible, repeatable pattern; keep movements small, smooth, and chest-quiet.
3. Breathe Through Your Nose, Quiet and Low
Nasal breathing supports diaphragmatic breathing by naturally slowing airflow, warming and humidifying the air, and encouraging low, quiet inhalations. It also helps you keep the mouth relaxed, which reduces the tendency to shrug or gasp. If you’re congested, do what’s comfortable, but return to nose-first as soon as you can. Keep the inhale silent or nearly so; noisy mouth inhalations often signal you’re pulling too hard or lifting the chest. The “feel” you’re after is gentle belly and rib expansion with minimal upper-chest movement and minimal sound.
3.1 How to do it
- Rest the tongue lightly on the palate; lips together, jaw relaxed.
- Imagine inhaling “down and wide” into the belly and low ribs.
- Exhale through the nose or pursed lips (whichever feels easier/longer).
3.2 Numbers & guardrails
- If you hear wheezing or feel breath hunger, reduce depth and slow down.
- If nasal breathing is difficult due to allergies or a cold, shorten sessions and keep effort easy until clear.
Synthesis: Nose-first, quiet air sets the conditions for low, diaphragm-led breaths and makes the relaxation effect more reliable.
4. Lengthen the Exhale and Choose a Cadence
A slightly longer exhale is a practical, safe way to downshift the nervous system. Start by matching inhale and exhale lengths (e.g., 4 in / 4 out), then make the exhale modestly longer (e.g., 4 in / 6 out). Most adults settle into 6–10 breaths per minute; many feel calm near ~6 breaths/min (about 5 seconds in, 5–7 seconds out). The aim isn’t “more air,” it’s smoother, slower air with an exhale that feels unhurried. If you strain to hold a long exhale, shorten it; comfort and repeatability beat perfection.
4.1 Practical cadences
- Even: 4–5 seconds in, 4–5 seconds out (great starting point).
- Exhale-weighted: 4 seconds in, 6–8 seconds out (calming for stress).
- Micro-pause: 4 in, 1–2 second soft pause, 6 out (optional).
4.2 Tools & examples
- Use a metronome app or the “Breathe/Respire” feature on smartwatches.
- Try free timers (e.g., Insight Timer) or breathing apps (e.g., Breathwrk, Calm, Headspace) to guide pacing.
Synthesis: Pick a cadence that feels smooth and sustainable; consistent, longer exhales—not bigger breaths—drive the calm you’re after.
5. Expand 360°: Belly, Ribs, and Back
Diaphragmatic breathing isn’t only “belly out.” The diaphragm moves downward and the lower ribcage widens in all directions—front, sides, and back. Think of a gentle 360° umbrella opening at your waistline. This distributes motion, reduces low-back and neck compensation, and makes the breath feel fuller with less effort. If you only push the belly forward, you can miss lateral rib movement; if you only expand the ribs, you may brace the abdomen. Balancing belly and rib motion creates a smooth, stable cylinder through your trunk.
5.1 How to do it
- Wrap a light elastic band, scarf, or your hands around the lower ribs.
- On inhale, feel gentle expansion into the band in front/sides/back.
- On exhale, feel the band soften evenly without collapsing posture.
5.2 Mini-checklist
- Belly moves some; ribs widen some; back expands a little.
- Chest and shoulders stay quiet; jaw stays easy.
- No breath-holding unless very brief and comfortable.
Synthesis: Aim for a 360° “umbrella” of expansion; balanced motion improves efficiency and keeps your neck and chest from doing the diaphragm’s job.
6. Add Gentle Resistance and Pacers
Once the pattern feels smooth, mild resistance can slow the exhale and enhance the calming effect. The simplest tool is a pursed-lip exhale—like blowing through a thin straw—which naturally lengthens outflow without forcing it. Pacers (visual, audio, or haptic cues) help you keep time without counting in your head. Think of these as training wheels that you can keep or discard depending on context. Keep resistance gentle; if the exhale feels pressured or you get dizzy, back off immediately.
6.1 Tools & examples
- Pursed-lip exhale: kiss-face lips, steady small stream of air.
- Box/timed breathing apps: set custom in/hold/out counts.
- HRV biofeedback: chest strap or camera-based apps visualize heart rhythms while you breathe.
- Low-tech: metronome at 6–7 ticks per 10 seconds; follow the beat.
6.2 Numbers & guardrails
- Keep perceived effort 2–4/10; never “push” air out.
- 2–5 minutes per session is plenty; quality beats quantity.
- Stop if you feel tingling/tinges of lightheadedness; return to normal breathing and resume later with shorter sessions.
Synthesis: Light resistance and simple pacers make slow, smooth exhales easier to repeat—use them to groove the pattern, not to force bigger breaths.
7. Progress from Floor to Movement
Skills stick when you can use them in more situations. Start on the floor (supine), then practice seated, then standing, and finally during gentle movement (e.g., walking). Each new position adds a little challenge to trunk control and breath rhythm; keep the same cues: belly and ribs expand; exhale is a touch longer; shoulders stay quiet. As you add movement, expect smaller excursions and shorter counts—that’s normal. The win is keeping the pattern under light activity without strain.
7.1 Progression roadmap
- Supine: 2–4 minutes, knees bent, hands on belly/ribs.
- Seated: 2–3 minutes at your desk, back away from chair back.
- Standing: 1–2 minutes, soft knees, easy sway.
- Walking: match 3–4 steps inhale, 4–6 steps exhale; keep it easy.
7.2 Common mistakes
- Holding posture rigid; allow small natural sway.
- Forcing the same long counts while moving; shorten to stay comfortable.
- Mouth breathing as intensity rises; return to nasal if possible.
Synthesis: Layer the skill into daily positions so it’s available when you need it most; adapt counts to the context and keep the pattern relaxed.
8. Build Micro-Habits and Stress Cues
Consistency beats intensity. Tie diaphragmatic breathing to daily anchors so you practice without thinking. Use tiny, frequent bouts—60–120 seconds—whenever you change tasks, wait for a download, or sit in a rideshare. The goal is automaticity: when stress hits, your body already knows what to do. Pairing the habit with visual or haptic reminders (phone widgets, watch prompts) helps keep the streak going without willpower.
8.1 Habit anchors to try
- First sit at your desk → 6 slow breaths.
- Calendar alert before meetings → 1 minute of exhale-weighted breathing.
- Park the car or close the laptop → 10 quiet breaths before moving on.
- Bedtime lights-out → 2–3 minutes of 4-in / 6–8-out.
8.2 Mini-checklist
- Keep sessions short, pleasant, and repeatable.
- Track “streaks” or minutes if you like data, but don’t chase numbers.
- If a day gets away from you, resume tomorrow—no punishment.
Synthesis: Micro-sessions attached to existing routines turn a technique into a lifestyle—so the skill shows up when stress does.
9. Apply Protocols for Work, Anxiety, and Sleep
Different situations call for small tweaks. For work focus, even-paced nasal breathing settles arousal without making you sleepy. For acute anxiety, longer, pursed-lip exhales can help you ride out the spike. For sleep, dim lights and exhale-biased breathing while lying on your side often shortens sleep-onset latency. All three share the same base: low, quiet, comfortable breaths with minimal upper-chest movement. Match the protocol to the moment, and keep sessions brief and repeatable.
9.1 Situation-specific templates
- Before a meeting (focus): 4 in / 4 out for 1–2 minutes, nasal only.
- During a stress spike (calm): 4 in / 6–8 out with pursed lips for 1–3 minutes; stop when you feel a notch calmer.
- At bedtime (downshift): Side-lying, 3–4 in / 6–7 out, lights low, 2–5 minutes.
9.2 Region & context notes
- In public transit or shared offices, keep breaths subtle and quiet—no visible “belly pumping.”
- If you wear a mask in clinics or transit, shorten counts and keep effort low; comfort first.
Synthesis: Choose a simple template for the task at hand—focus, calm, or sleep—and keep the same low, quiet mechanics across contexts.
10. Track, Iterate, and Stay Safe
Tracking helps you notice benefits and troubleshoot snags. A simple log of minutes practiced, perceived stress (0–10), and sleep quality is enough. If you enjoy gadgets, HRV-tracking wearables or smartphone apps can visualize changes; just don’t let data displace the feeling of calm. Safety is straightforward: avoid over-breathing, stop if dizzy, and consult a clinician if you have respiratory/cardiac issues or persistent symptoms. Progress comes from gentle consistency—not from chasing extreme breath holds or huge volumes.
10.1 What to track
- Inputs: minutes practiced, contexts (desk, commute, bedtime).
- Outputs: stress ratings, ease falling asleep, perceived calm post-session.
- Optional: resting heart rate or HRV trends if you use a device.
10.2 Troubleshooting
- Dizzy/tingly: you’re likely breathing too big/fast → shrink the breath and slow down.
- Neck tightness: chest is leading → return to hand placement and soften shoulders.
- Can’t feel belly move: loosen waistband, try supine, or add a light book over the belly for feedback.
Synthesis: Measure what matters, adjust gently, and prioritize safety; a small, sustainable practice beats a perfect but fragile one.
FAQs
1) What exactly is diaphragmatic breathing, in one sentence?
It’s a calm, low, mostly nasal breathing pattern where the diaphragm does the work—your belly and lower ribs expand on the inhale and soften on the exhale—used to reduce stress and steady your physiology. The technique favors smooth, comfortable breaths rather than big or forced breaths, which helps you relax without getting dizzy.
2) How long should each practice session be, and how often?
Most people do well with 2–5 minutes per session, 2–4 times per day, plus as-needed “micro-bouts” before stressful moments. That’s long enough to feel a tangible shift without fatigue. If you’re brand new or get lightheaded, start with 60–90 seconds and build up slowly over a week or two.
3) Is this the same as “belly breathing”?
“Belly breathing” is a common cue that helps you find the diaphragm, but true diaphragmatic breathing includes the lower ribs and back expanding slightly as well. Think 360°, not just belly out. If you only push your stomach forward, you may miss the gentle widening of the ribcage that makes the pattern efficient and comfortable.
4) Should I breathe in through my nose and out through my mouth?
Nasal inhalations are ideal because they slow and condition airflow. For the exhale, use the nose or gently pursed lips—whichever helps you lengthen the exhale without strain. If you’re congested or exercising, do what’s comfortable and return to nose-first as soon as feasible.
5) What cadence is best for stress relief?
Many people feel calm near 6–10 breaths per minute (for example, 4 seconds in and 6–8 seconds out). There is no single magic number; choose a cadence that is smooth and repeatable. If counting feels stressful, use a visual or audio pacer and aim for a slightly longer, easy exhale.
6) Can diaphragmatic breathing help with anxiety or panic?
It can be a helpful tool—not a cure. When anxiety spikes, use brief sets of exhale-weighted breathing (e.g., 4 in / 6–8 out) and keep attention on the feeling of air leaving. This can reduce the intensity of the moment while you use other supports (movement, grounding, therapy tools). If panic attacks are frequent or severe, seek professional care.
7) Is it safe for people with asthma, COPD, or during pregnancy?
Many clinicians teach diaphragmatic breathing in rehabilitation and prenatal care, but individual needs vary. If you have asthma, COPD, cardiac issues, are pregnant, or experience breathlessness, consult your clinician first. Stay within comfortable ranges, avoid forcing long breath holds, and stop if you feel unwell.
8) Will this lower my blood pressure or improve HRV?
Slow, comfortable breathing often leads to lower heart rate and steadier heart-rhythm patterns in the moment, and some people see favorable trends over time. Responses vary, and devices/apps can help you notice your own patterns. Use these metrics as gentle feedback rather than goals to chase.
9) How is this different from 4-7-8 or box breathing?
Those are timing protocols; diaphragmatic breathing is the mechanic behind them. If you can keep breaths low, quiet, and exhale-weighted, you can plug many timing patterns on top. For stress relief, choose counts you can sustain smoothly rather than rigidly chasing a specific formula.
10) What if I feel more anxious when I focus on my breath?
That’s common at first. Shrink the breath, shorten sessions to 30–60 seconds, and switch attention to gentle sensations (e.g., hands on ribs or the feel of air at the nostrils). You can also hum lightly on the exhale to keep it slow without over-focusing on numbers. Build up gradually as comfort grows.
11) Can I use diaphragmatic breathing during exercise or recovery?
Yes—with modifications. During light movement, keep nasal, low, quiet breaths; as intensity rises, you may naturally switch to mixed mouth/nose breathing. After workouts, 2–3 minutes of exhale-biased nasal breathing can speed the shift into recovery without making you sleepy.
12) Which apps or tools are worth trying?
You don’t need any, but pacer/timer apps (e.g., Breathwrk, Calm, Headspace), a simple metronome, or smartwatch breathing prompts can help you lock in cadence. If you like data, HRV apps and wearables can visualize patterns; treat them as feedback, not a score to win.
Conclusion
Diaphragmatic breathing is a simple, portable skill: low, quiet inhalations that expand the belly and lower ribs, followed by unhurried exhales that gently outlast the inhale. With a supportive posture, hand feedback, nasal airflow, and a cadence you can repeat without strain, you can cue your body to settle in just a few minutes. The real power comes from consistency—short, pleasant bouts tied to daily anchors like pre-meeting pauses, commute transitions, and lights-out. As you progress from floor to standing to gentle movement, you’ll discover the pattern holds even when life gets noisy. Keep sessions easy, track what matters to you (stress, sleep, mood), and adjust gently when something feels off. Start small today: six quiet breaths, exhale a little longer than you inhale, and notice the notch of calm arrive. Ready to try? Take 60 seconds now and do six exhale-weighted breaths.
References
- Diaphragmatic Breathing: Techniques & Benefits, Cleveland Clinic, 2023, https://my.clevelandclinic.org/health/articles/9445-diaphragmatic-breathing
- Breathing exercises for stress, NHS, 2021, https://www.nhs.uk/mental-health/self-help/guides-tools-and-activities/breathing-exercises-for-stress/
- Breathing Exercises, American Lung Association, 2022, https://www.lung.org/lung-health-diseases/wellness/breathing-exercises
- Relaxation techniques: Breath control helps quell the chaos of stress, Harvard Health Publishing, 2020, https://www.health.harvard.edu/mind-and-mood/relaxation-techniques-breath-control-helps-quell-chaos-of-stress
- Ma X., Yue Z., Gong Z. et al., The Effect of Diaphragmatic Breathing on Attention, Negative Affect and Stress in Healthy Adults, Frontiers in Psychology, 2017, https://doi.org/10.3389/fpsyg.2017.00874
- Relaxation Techniques: What You Need To Know, National Center for Complementary and Integrative Health (NCCIH), 2019, https://www.nccih.nih.gov/health/relaxation-techniques-what-you-need-to-know
- Deep breathing, MedlinePlus Medical Encyclopedia, 2024, https://medlineplus.gov/ency/article/002241.htm
- Lehrer P. & Gevirtz R., Heart Rate Variability Biofeedback: How and Why Does It Work?, Applied Psychophysiology and Biofeedback, 2014, https://link.springer.com/article/10.1007/s10484-014-9248-9