Stress and anxiety are part of being human—but how you think about them can change how strongly they affect you. This guide focuses on managing stress and anxiety with a healthy mindset using eight practical, science-backed approaches you can start today. You’ll learn how to reframe pressure as a challenge, calm your body with breath and movement, sleep better, and support your mind with proven tools from cognitive and mindfulness-based therapies.
Quick answer: Managing stress and anxiety with a healthy mindset means reframing threats as challenges, practicing skills that regulate your body (breath, sleep, movement), and using evidence-based thinking tools to respond—not react—to stressors.
Important: This article is educational and not a medical diagnosis or treatment plan. If you’re in crisis or thinking about self-harm, seek immediate help. In Pakistan, the government’s Humraaz/1166 mental health helpline is available; globally, see findahelpline.com for local support.
Fast start (5 steps):
- Pause and breathe slowly through your nose for 2–5 minutes.
- Name the stressor and the feeling (“I’m anxious about tomorrow’s presentation”).
- Reframe: “This is my body gearing up to help me perform.”
- Take one small action that reduces uncertainty (e.g., outline slides).
- Close the loop: a short walk, stretch, or a warm shower to reset.
1. Reframe Stress with Cognitive Reappraisal
Reframing stress works by changing the story you tell yourself about what’s happening, which changes the emotion that follows. In cognitive reappraisal, you reinterpret a stressful event (e.g., “I might bomb this interview”) as something more accurate and helpful (“Interviews are challenging, but I’ve prepared—this is a chance to tell my story”). This isn’t toxic positivity; it’s a deliberate, realistic shift that reduces threat while preserving motivation. Robust evidence shows reappraisal is associated with better mental health, greater resilience, and lower stress responses across populations. Think of it as upgrading the lens you use—same situation, clearer view, calmer body.
1.1 Why it matters
- A 2024 meta-analysis shows reappraisal skills protect against stress and adversity, strengthening resilience.
- Reappraisal changes underlying appraisals that generate negative emotion, a core mechanism described in emotion regulation research.
1.2 How to do it (mini-checklist)
- Name it: “I’m feeling anxious about X.”
- Ask for evidence: “What facts support my fear? What contradicts it?”
- Generate alternatives: Two plausible, less catastrophic explanations.
- Choose a helpful thought: One that’s accurate and goal-aligned.
- Anchor in action: Identify the next concrete step (email, outline, call).
1.3 Common mistakes
- All-or-nothing thinking: Replace with graded language (“some,” “often,” “yet”).
- Over-reassurance seeking: Balance with self-reassurance + small actions.
- Skipping behavior: Reappraisal lands best when paired with doing.
Bottom line: Reappraisal is a learnable, repeatable skill that transforms stress from an enemy into information you can use.
2. Train Attention with Mindfulness (MBSR & Everyday Mindfulness)
Mindfulness builds the capacity to notice thoughts and sensations without immediately fighting or following them. That space is powerful: anxiety loses its grip when you can observe it and re-orient to what matters. Standard programs like Mindfulness-Based Stress Reduction (MBSR)—often 8 weeks—have demonstrated improvements in anxiety, mood, and well-being; newer online versions broaden access while showing promising outcomes. You don’t need a retreat: 10–15 minutes daily, plus “micro-practices” during the day, can shift reactivity into steadiness.
2.1 How to get started
- Set a tiny habit: 10 minutes after lunch, sit, breathe, and note sensations.
- Use guided audio: WHO’s Doing What Matters in Times of Stress has brief exercises rooted in acceptance-based skills. The MHPSS Network
- Bring mindfulness to tasks: One mindful shower, one mindful email, one mindful walk daily.
2.2 Numbers & guardrails (as of August 2025)
- 8-week MBSR has repeatedly shown anxiety reductions; online formats also report moderate effects in clinical and occupational groups.
- Expect early benefits (more awareness, fewer spirals) in 2–3 weeks; skills compound with consistency.
2.3 Tools/Examples
- Apps with 10-minute sessions; alarms that say “Pause for 3 breaths”; a sticky note on your monitor: “Notice. Name. Allow.”
Bottom line: Mindfulness strengthens the “pause button” between trigger and reaction, making room for wiser choices under stress.
3. Calm the Body with Slow Breathing & HRV-Friendly Practices
Your nervous system has a “brake” (parasympathetic) and a “gas” (sympathetic). Slow, diaphragmatic breathing nudges the brake—lowering heart rate and easing anxious arousal. Reviews and meta-analyses show breathwork can reduce perceived stress and improve mood, likely by boosting vagal tone and synchronizing brain rhythms with respiration. Short bouts (2–5 minutes) scattered through the day can be surprisingly effective, especially before known stressors (presentations, tough conversations).
3.1 Mini-protocols you can use anywhere
- Box/Nasal breathing: In 4, hold 4, out 4, hold 4; repeat for 2–3 minutes.
- Extended exhale: In 4, out 6–8 (gently); 3–5 minutes before bed.
- “Physiological sigh” sets: Two quick nasal inhales + long exhale; 1–2 minutes to reduce acute tension.
3.2 Numbers & guardrails
- Start with 2–5 minutes, 2–3 times daily; consistency beats intensity.
- If you feel light-headed, pause and return to natural breathing.
- Pair breathwork with body awareness: one hand on chest, one on belly.
3.3 Tools/Examples
- Phone timer labeled “Breathe.”
- HRV-biofeedback devices/apps can guide pace and track progress.
Bottom line: Slow breathing is a portable de-stressor that teaches your body a calmer default—no equipment required.
4. Move Your Body: Exercise as an Anti-Anxiety Dose
Regular physical activity is a potent mood regulator. Meta-analyses of randomized trials report moderate effects of exercise on depressive symptoms and meaningful benefits for anxiety; combined aerobic and resistance training performs well. For mental health and overall well-being, adults should aim for 150–300 minutes/week of moderate-intensity or 75–150 minutes/week of vigorous activity, plus 2+ days/week of muscle-strengthening—targets backed by WHO and national guidelines. Start where you are: brisk walking counts, and short bouts add up.
4.1 How to do it (starter plans)
- Low-time option: 3×/week 25-minute brisk walks + 2×/week 10-minute body-weight circuits.
- Balanced option: 2 days full-body resistance (30–40 min) + 2 days cycling/jogging (20–30 min).
- Micro-bursts: 5-minute “movement snacks” (stairs, squats, pushups) between meetings.
4.2 Numbers & guardrails (as of August 2025)
- WHO’s guideline range gives most benefits; go beyond gradually if desired.
- Aim for RPE 5–7/10 on cardio days; keep strength sets 2–4 per muscle group.
- If deconditioned or managing a condition, clear new programs with your clinician.
4.3 Common roadblocks & fixes
- All-or-nothing: Use “minimums”: 10 minutes today still counts.
- Boredom: Rotate modalities; pair workouts with music/podcasts.
- Time: Tie habits to anchors—after school drop-off, during lunch, after prayer.
Bottom line: Movement is medicine for mood—dose it like a prescription, consistently, and your mind will feel the lift.
5. Protect Sleep to Break the Stress–Anxiety Loop
Sleep and anxiety feed each other: worry disrupts sleep, and poor sleep heightens stress reactivity the next day. Prioritizing 7+ hours with consistent bed/wake times improves emotion regulation and coping capacity; behavioral treatments like CBT-I (sleep restriction, stimulus control, relaxation) are first-line for chronic insomnia and help reduce anxiety symptoms linked to poor sleep. Build a wind-down routine, dim evening light, and keep caffeine earlier in the day. When sleep improves, stress feels less like a wave and more like a ripple. CDC
5.1 Sleep upgrades (mini-checklist)
- Same schedule: ±30 minutes, even on weekends.
- Wind-down: 60–90 minutes of low-stimulation routine.
- Light & screens: Dim lights after sunset; avoid bright screens near bedtime.
- Caffeine/alcohol: Cut caffeine after early afternoon; limit alcohol in the evening.
- Bedroom: Cool, dark, quiet; bed for sleep and intimacy only.
5.2 When to seek help
- If insomnia persists 3+ nights/week for 3 months, talk to your clinician; ask about CBT-I or reputable digital CBT-I programs.
Bottom line: Guarding sleep is a high-leverage investment: better rest = steadier mood, clearer thinking, and more stress resilience. Harvard Sleep Medicine
6. Release Tension with Progressive Muscle Relaxation (PMR)
Anxiety often shows up as a tight jaw, stiff shoulders, or a churning stomach. Progressive Muscle Relaxation (PMR) systematically tenses and releases muscle groups to downshift the body’s alarm system. Trials and reviews report PMR reduces stress and anxiety across settings, and it pairs well with other interventions like CBT, mindfulness, or breathwork. PMR is simple: 10–15 minutes, a quiet spot, and a guided script can reset your baseline tension—especially useful before bedtime or after a draining day. PubMed
6.1 How to do it (head-to-toe)
- Sit or lie down; inhale while gently tensing a muscle group for ~5 seconds.
- Exhale and release for ~10 seconds, noticing the contrast.
- Move from feet → calves → thighs → glutes → belly → chest → hands → arms → shoulders → neck → face.
6.2 Numbers & guardrails
- Practice 3–4 times/week for 2–4 weeks, then use as needed.
- Keep tension moderate—no pain, cramps, or holding breath.
- Combine with extended exhale breathing to deepen relaxation.
6.3 Common mistakes
- Rushing; skipping body awareness; straining small muscles (jaw/neck).
Bottom line: PMR teaches your body what “relaxed” feels like, so you can return there more quickly under stress.
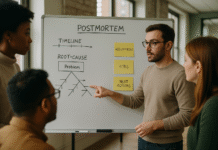
7. Face Fears Gradually: Exposure, Acceptance & “Doing What Matters”
Avoidance gives short-term relief but long-term anxiety. Gradual, values-guided exposure helps you learn you can cope. Acceptance and Commitment Therapy (ACT) adds a compass: clarify what matters, accept uncomfortable feelings, and take small, committed actions anyway. WHO’s Doing What Matters in Times of Stress distills these ideas into brief, field-tested exercises you can practice daily, with facilitator-led versions (Self-Help Plus) also available in many regions. Start tiny, go slow, and let confidence grow from experience.
7.1 How to do it (graded plan)
- List triggers: Rank 0–10 for anxiety intensity.
- Design steps: Break one trigger into 5–8 rungs, from easiest to hardest.
- Practice: Work each rung until anxiety drops ≥50% or feels manageable.
- Reflect: Record what you learned; celebrate progress.
7.2 Tools/Examples
- For social anxiety: Step 1—make brief eye contact with a barista; Step 2—ask a simple question; Step 3—short conversation; Step 4—join a small meeting comment, etc.
- Audio supports: Free ACT-style grounding audios can help you practice “dropping anchor” when anxiety spikes.
Bottom line: Exposure plus acceptance breaks avoidance cycles and reconnects you to a life guided by values—not fear.
8. Strengthen Support, Priorities, and Daily Habits
Humans regulate stress socially. Consistent social support predicts lower perceived stress and fewer anxiety symptoms; even brief check-ins help. Pair support with clear priorities (say “no” when bandwidth is gone), gratitude practices, and simple self-care habits like regular meals and movement. Many of these habits appear in national mental-health guidance because they reliably shift people back to steadier ground, especially during demanding seasons at work or home. If you need structured backing, community groups and helplines can connect you with trained listeners in your area.
8.1 Practical moves (this week)
- Two-by-two: Two 15-minute connection calls; two 10-minute walks.
- Priorities list: Must-do, should-do, could-do; schedule the musts.
- Gratitude cue: Write three specifics at the same time daily (e.g., after dinner).
- Boundaries: One kind “no” to protect sleep or recovery.
8.2 Region-specific notes (Pakistan + global)
- Pakistan’s Humraaz/1166 initiative offers mental-health support via helpline and app; local NGOs such as Taskeen also provide telephonic support. Global readers can use findahelpline.com for verified services. TaskeenFind A Helpline
Bottom line: Supportive relationships and clear priorities reduce load on your nervous system—turning chronic strain into manageable challenge.
FAQs
1) What’s the fastest way to feel calmer before a stressful event?
Two to five minutes of slow, nasal, diaphragmatic breathing (or several “physiological sighs”) can quickly reduce autonomic arousal. Pair it with a brief reframe: “My body is mobilizing energy to help me focus.” Practicing daily makes the effect stronger and more reliable when you need it.
2) Is mindfulness just “clearing the mind”?
No. Mindfulness is paying attention, on purpose, to present-moment experience with curiosity and non-judgment. You’ll still have thoughts—mindfulness changes your relationship to them. Programs like MBSR (including online options) show measurable anxiety and stress reductions when practiced consistently. PMCBioMed Central
3) How much exercise helps anxiety?
Even small amounts help, but guidelines suggest 150–300 minutes/week of moderate activity or 75–150 minutes/week of vigorous activity, plus 2+ strength days. Meta-analyses show exercise meaningfully improves mood; mix cardio and resistance for best results.
4) I sleep poorly when stressed. What should I try first?
Protect a consistent sleep window, add a 60–90-minute wind-down, dim screens and lights near bedtime, and limit late caffeine. If insomnia persists, talk to your clinician about CBT-I or reputable digital CBT-I programs; these have strong evidence. CDC Blogs
5) Are supplements necessary?
Most people don’t need supplements solely for stress/anxiety, and they can interact with medications. Focus first on breathwork, movement, sleep, and cognitive skills. Discuss any supplement use with a qualified clinician, especially if you’re pregnant, nursing, or have medical conditions. (General guidance; consult your provider.)
6) What if reframing feels fake?
Reframes must be credible. You’re not forcing positivity; you’re seeking a more accurate, helpful angle. If that’s hard, try “both/and” statements (“I feel anxious, and I’m prepared”), or pair reappraisal with one small action to reinforce the new story.
7) Does progressive muscle relaxation really help?
Yes. Studies across populations show PMR reduces stress and anxiety, and it can improve sleep when practiced regularly. It’s safe, low-cost, and complements other approaches like CBT and mindfulness.
8) How do I stop avoiding things that make me anxious?
Use graded exposure: break a feared situation into steps from easiest to hardest, practice each step until anxiety drops, and move up gradually. ACT-style tools (like WHO’s Doing What Matters) provide simple exercises to support this work. Consider professional guidance for complex fears.
9) What free resources can I try today?
WHO’s Doing What Matters guide and audio, national mental-health pages (e.g., NIMH), and some ACT audio practices are free. Many local helplines can also direct you to services at low or no cost. Act Mindfully
10) When should I seek professional help?
If anxiety disrupts work, relationships, or sleep for several weeks; if you’re using alcohol or substances to cope; or if you have panic attacks, intrusive thoughts, or any self-harm thoughts—contact a licensed professional. In emergencies, use local crisis lines (e.g., 1166 in Pakistan) or your country’s emergency number.
Conclusion
Managing stress and anxiety with a healthy mindset is less about eliminating pressure and more about changing your stance toward it. When you reframe challenges, train attention, calm your physiology, move your body, and protect sleep, your nervous system learns a steadier baseline. Skills like PMR and values-guided exposure help you act even when discomfort is present, while social support and clear priorities reduce load and amplify resilience. You don’t need to master everything at once. Pick one or two strategies—perhaps slow breathing plus a nightly wind-down—and practice them daily for two weeks. Then layer in reappraisal or a movement routine. Over time, you’ll build a personal toolkit that makes stress manageable and life more aligned with what matters.
Start today: Schedule two 5-minute breath breaks and a 60-minute earlier lights-down tonight.
References
- Stover AD, et al. A meta-analysis of cognitive reappraisal and personal resilience. Clinical Psychology Review. 2024. PubMed
- Troy AS, et al. Cognitive Reappraisal and Acceptance: Effects on Emotion. Perspect Psychol Sci. 2018 (article archived 2017/2018). PMC
- Bentley TGK, et al. Breathing Practices for Stress and Anxiety Reduction. Ann N Y Acad Sci. 2023. PMC
- Fincham GW, et al. Effect of breathwork on stress and mental health: Meta-analysis. Sci Rep. 2023. Nature
- Noetel M, et al. Effect of exercise for depression: Systematic review and meta-analysis of RCTs. BMJ. 2024. BMJ
- World Health Organization. 2020 Guidelines on Physical Activity and Sedentary Behaviour. 2020. PMC
- Edinger JD, et al. Behavioral and psychological treatments for chronic insomnia disorder in adults: AASM guideline. J Clin Sleep Med. 2021. PMC
- Khir SM, et al. Efficacy of Progressive Muscle Relaxation in Adults for Stress, Anxiety, and Depression. Psychol Res Behav Manag. 2024. PMC
- World Health Organization. Doing What Matters in Times of Stress: An Illustrated Guide. 2020–2021 (guide and audio). World Health Organization
- DawN (Pakistan). Mental health app, helpline launched (Humraaz/1166). Apr 8, 2023. Dawn
- National Institute of Mental Health (NIMH). Caring for Your Mental Health. 2024 update. National Institute of Mental Health
- Acoba EF, et al. Social support and mental health: mediating role of perceived stress. Front Psychol. 2024. https://www.frontiersin.org/articles/10.3389/fpsyg.2024.1330720/full Frontiers
- American CDC. Managing Stress | Mental Health. 2025. CDC
- American Academy of Sleep Medicine. Digital CBT-I platforms and characteristics. 2024. AASM