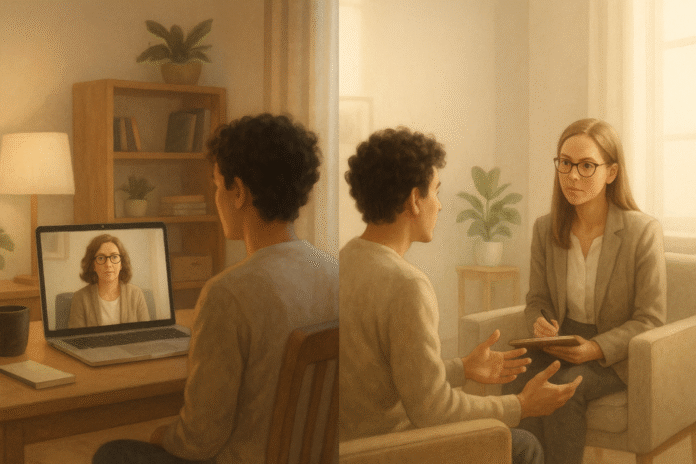
Finding the right balance between online vs. in-person support can turn “I hope this helps” into “I know what works for me.” This guide is for anyone weighing therapy, coaching, peer groups, or community support across screens and rooms. In short: online support matches in-person outcomes for many common needs and dramatically improves access; in-person still excels when safety, complexity, or hands-on work are central. A smart hybrid plan combines the two so you get convenience without sacrificing connection. (Educational, not medical advice. If you’re in crisis, seek local emergency care immediately.) Evidence from recent reviews shows telehealth psychotherapy is generally comparable to in-person care for depression and anxiety, with no meaningful differences in symptom reduction or dropout—a strong signal that you can choose based on fit, not fear.
1. Decide by Goal and Risk, Not by Hype or Habit
Start by matching the format to your immediate goal and safety needs: choose in-person when risk is high or assessment is complex; choose online when access, scheduling, or stigma barriers would otherwise delay care. For many routine therapy goals (e.g., CBT for depression/anxiety), research finds teletherapy achieves similar outcomes to in-person, so you can prioritize logistics and preference without sacrificing effectiveness. If your situation involves active suicidality, unstable medical or psychiatric conditions, or domestic safety concerns, start in person (or a higher level of care) and use online adjuncts later. The key is to anchor the decision to your goals—symptom relief, skill-building, social connection—and to adjust as your goals evolve over time.
1.1 How to triage your first step
- High risk/complexity: start in person (or intensive program); add online check-ins after stabilization.
- Moderate, skills-based goals: either format is viable; choose the one you’ll actually attend.
- Access barriers (distance, disability, caregiving): prioritize online, then layer periodic in-person sessions.
- Group/community connection: pick the format your target group sustains (cohesion > modality).
- Privacy constraints at home: lean in person until you can secure a private online setting.
1.2 Mini example
A graduate student with panic attacks and a 60-hour week opts for online CBT to start (flexibility), then schedules monthly in-person sessions ahead of exams. Symptoms drop within eight weeks; they keep one quarterly in-person booster for accountability. A goals-first approach keeps the plan practical and safe. Evidence supports equivalence for common conditions, so fit and feasibility can lead.
Bottom line: Let goals and risk decide format; when risk is low, choose the modality you can sustain.
2. Build a Hybrid Plan You’ll Actually Use
A hybrid plan—some sessions online, some in person—often delivers the best of both worlds. Start with the channel that removes the biggest barrier (usually online for speed of access), then add in-person sessions to deepen the relationship, practice exposure tasks, or navigate nuanced conversations. Studies during and after the pandemic show teletherapy outcomes are noninferior to in-person for many diagnoses, suggesting you can flex between channels without losing progress. Treat the hybrid plan like a program with milestones, scheduled reviews, and clear rules for when to switch.
2.1 How to structure a 12-week hybrid
- Weeks 1–2: two online sessions/week for momentum and psychoeducation.
- Weeks 3–6: weekly online; add one in-person session to practice a feared task (e.g., exposure).
- Weeks 7–10: alternate online and in person; introduce a group (online or local) for peer support.
- Weeks 11–12: taper to online biweekly; schedule an in-person review with outcome measures.
2.2 Numbers & guardrails
- Cadence: aim for ≥75% session adherence; reschedule within 7 days if you cancel.
- Switch rules: if PHQ-9 or GAD-7 worsens by ≥5 points for two checks, insert an in-person review.
- Ceiling: if you miss 3 sessions in a row online, convert next two to in person.
2.3 Why hybrid works
The therapeutic alliance—a strong predictor of outcome—shows parity across modalities when therapists apply good teletherapy skills. That means you can preserve relationship quality while optimizing logistics.
Bottom line: Hybrid gives you flexibility with depth; set explicit cadence, metrics, and switch rules.
3. Protect Privacy, Data, and Legal Basics Before You Click “Join”
Privacy isn’t just a preference; it’s a prerequisite. Before starting online support, verify platform security (end-to-end encryption, access controls), understand data handling (who can access recordings or chat logs), and create a private physical setting. Professional bodies outline standards for telepsychology—covering consent, emergency planning, jurisdiction, and documentation—that your provider should follow. You’re also responsible for your side: secure Wi-Fi, headphones, and a session routine that avoids interruptions. In-person sessions do not eliminate privacy risks (e.g., being seen at a clinic), but they shift them from data security to physical discretion.
3.1 Mini-checklist (client side)
- Consent: read and sign telehealth consent; note emergency procedures and your location at each session.
- Setup: use a private room, white noise, and headphones; disable smart speakers.
- Devices: update OS/browser; lock screen with a passcode; avoid public Wi-Fi.
- Platform: prefer vendor-provided app/browser links; avoid recording unless explicitly agreed.
- Backups: share a secondary contact and local crisis resources with your provider.
3.2 Provider standards to expect
- Clear identification, licensure and jurisdiction boundaries.
- Secure platform vetted for clinical use; documented risk protocols.
- Transparent data retention and no unauthorized recording.
- Contingency plan for outages (phone backup, reschedule rules).
- Location check each session for emergency dispatch.
Authoritative guidance (e.g., APA telepsychology revisions; APA/ATA telepsychiatry resources) sets these expectations and is updated periodically. Ask your provider how they implement them.
Bottom line: Treat privacy and safety as shared responsibilities; confirm standards before your first online session.
4. Make Online Sessions Feel “Real”: Alliance and Presence Skills
Online conversations can feel flat—unless you deliberately create social presence. The first minute sets tone: camera at eye level, stable lighting, clear audio, and an arrival ritual (deep breath, agenda, goals). Research indicates therapeutic alliance in teletherapy is noninferior to in-person when clinicians are trained and intentional, and that perceived presence can be engineered through simple choices in framing, pacing, and response time. Translate small in-room behaviors to the screen: visible note-taking, explicit empathy, intentional pauses, and shared documents for exercises.
4.1 Tools & micro-behaviors that lift presence
- Framing: eye-level camera, face centered; avoid backlighting.
- Bandwidth: wired or near-router connection; close all heavy apps.
- Rituals: 60-second check-in, recap last action step, set a single session goal.
- Transparency: narrate what you’re doing (“I’m pulling up your worksheet”).
- Buffers: 5-minute “settle” period at start and a 3-point summary at end.
4.2 Why it matters (theory meets practice)
Social Presence Theory (Short, Williams & Christie) explains why richer cues (eye contact, immediacy) enhance connection. You can’t replicate a room, but you can approximate immediacy with camera placement, vocal warmth, and quick feedback loops—enough to preserve alliance quality online. Recent meta-analyses show alliance remains a meaningful predictor of outcome in teletherapy.
Bottom line: Presence is a skill, not a place; small technical and relational choices protect the alliance online.
5. Choose the Right Group: Cohesion Online vs. In Person
Group support—therapy, coaching, or peer communities—works when cohesion, norms, and safety are strong. Online groups can match in-person results for many aims, but facilitators must work harder to manage turn-taking, side chats, and “Zoom fatigue.” If you need structured skills (e.g., CBT, mindfulness), online groups are often ideal; if you seek experiential work (e.g., somatic processing), in-person may be better. Evaluate a group by its onboarding, rules, and facilitation style—not just where it meets.
5.1 What predicts a good online group
- Clear tech norms: camera/microphone expectations, hand-raise, chat boundaries.
- Small size: 6–10 members improves airtime and cohesion.
- Stable roster: rolling admission lowers cohesion; fixed cohorts build safety.
- Practice time: breakout exercises with clear prompts.
- Asynchronous hub: shared docs/forum for between-session tasks.
5.2 Evidence snapshot
Systematic reviews find online group psychotherapy feasible and effective across conditions, with comparable outcomes to face-to-face in many studies; therapists note unique challenges (managing energy, fostering intimacy) that can be mitigated with structure. American Psychological Association
Bottom line: Pick groups on cohesion mechanics (size, rules, facilitation), not just modality.
6. Improve Access and Equity Without Lowering the Bar
Online support can be a lifeline for rural communities, people with disabilities, caregivers, and those juggling multiple jobs; it shrinks travel time and stigma. But access isn’t equity: bandwidth, language, disability accommodations, and digital literacy still shape outcomes. Health systems and global bodies emphasize standards for digital health so scale doesn’t outrun safety. Ask providers about captions, interpreters, screen-reader compatibility, and low-bandwidth options. If your region has public services (e.g., NHS Talking Therapies in England), ask what digital and in-person options exist and how outcomes are monitored.
6.1 Equity checklist
- Language: interpreter or bilingual clinician available online/in person.
- Accessibility: captions, transcripts, screen reader support.
- Bandwidth plan: audio-first fallback; phone backup with structured check-in.
- Cost: sliding scale, public options, or digital therapies recommended by national bodies.
- Outcomes: see real monitoring (PHQ-9/GAD-7) and recovery rates by modality.
6.2 Policy & systems notes
The WHO’s digital health strategy underscores building safe, equitable infrastructure; national programs like NHS Talking Therapies monitor outcomes at scale and increasingly integrate digital pathways—evidence you should expect measurement and options, not a one-size approach.
Bottom line: Demand accessibility features and transparent outcomes so online convenience doesn’t come at equity’s expense.
7. Use Evidence-Based Digital Tools (and Ditch the Noise)
Not all apps and programs are created equal. Internet-delivered CBT (iCBT) and videoconference-based CBT have strong evidence for depression and anxiety—especially when guided by a clinician or coach. Look for programs recommended or evaluated by reputable bodies; avoid tools that overpromise or hide data practices. Use digital tools to extend care between sessions: mood logs, exposure diaries, or relapse-prevention plans. Pair these with periodic in-person reviews to keep your plan anchored.
7.1 What to look for
- Evidence: RCTs or meta-analyses showing symptom reduction; guided > unguided.
- Transparency: clear privacy policy; data export/opt-out options.
- Interoperability: can share data with your clinician securely.
- Fit: brief (10–15 min/day), skill-oriented modules with reminders.
7.2 Evidence snapshot & practical tip
Meta-analyses and network analyses show iCBT and videoconference CBT are effective, with guided formats outperforming unguided ones. In 2024–2025, NICE and others recommended several digitally enabled therapies within stepped-care systems—use those lists to sanity-check vendors. If you’re starting unguided, schedule a five-minute weekly accountability text with a friend or coach; adherence often drives benefit. NICE
Bottom line: Choose validated, guided digital tools to augment sessions; let evidence, not gloss, guide you.
8. Draw Clear Red Lines: When Online Isn’t Enough
Some situations require in-person evaluation or higher levels of care, regardless of online convenience. If you’re experiencing active suicidal intent, recent self-harm, psychosis, uncontrolled substance withdrawal, or unsafe living conditions, seek emergency or urgent in-person care. Online sessions can still help after stabilization, but they should not delay hands-on assessment, labs, or safeguarding. Your provider should maintain an emergency plan and verify your current location at each online session so responders can reach you if needed.
8.1 A simple crisis plan to prepare now
- List your local emergency number and nearest emergency department.
- Add a trusted contact who can meet you or share your location.
- Know national/regional crisis lines (and text/chat options).
- Share your plan and physical address with your provider.
- Practice a “safe stop” protocol: how to pause an online session and seek immediate help.
8.2 Why the red lines exist
Reviews of telehealth in behavioral health show comparable outcomes and no increase in adverse events overall, but that assumes appropriate triage and escalation paths—your safety net should be explicit. If an online provider cannot tell you how they’d respond to a crisis where you are, that’s a signal to switch.
Bottom line: Name your red lines and crisis steps in advance; escalate to in-person care when safety is in play.
9. Measure Progress and Iterate (Data Beats Vibes)
Whether online or in person, measurement keeps you honest and helps you pivot early. Use brief, validated scales (e.g., PHQ-9 for depression, GAD-7 for anxiety) every 2–4 weeks; track adherence, session attendance, and one functional metric (sleep hours, missed workdays, or social activities). Hybrid plans benefit from “switch triggers” (e.g., worsening by ≥5 points or stalled improvement for a month). Health systems that scaled access (like NHS Talking Therapies) built routine outcome monitoring into care; you can, too.
9.1 A lightweight metrics stack
- Symptoms: PHQ-9/GAD-7 every other week (auto-scored forms).
- Function: 1–2 personal KPIs (e.g., 7 hours sleep/night; 2 social plans/week).
- Process: attendance rate, homework completion, self-efficacy rating.
- Review: 10-minute monthly “metrics huddle” with your provider.
9.2 Case example
You begin online CBT with PHQ-9 = 16. After four weeks, you’re at 10 (good), but GAD-7 is flat at 14. You and your therapist add one in-person session to rehearse a presentation exposure; two weeks later, GAD-7 drops to 9. This is how data—paired with hybrid flexibility—shortens the path to relief. National programs and manuals emphasize outcome monitoring; ask to see yours plotted over time.
Bottom line: Track a few metrics, review monthly, and let data trigger smart modality switches.
FAQs
1) Which is “better,” online or in-person support?
Neither wins in every case. For many common goals (CBT for depression/anxiety), teletherapy is as effective as in-person—so choose based on access, privacy, and comfort. For higher-risk or complex presentations, start in-person and add online later. The best answer is usually a hybrid that adapts as your needs change.
2) How do I know if my online provider is following standards?
Ask about licensure in your location, informed consent for telehealth, data security, emergency plans, and how they document your physical location each session. Professional guidelines detail these basics; providers should explain how they comply in plain language.
3) Do online groups actually work?
Yes—when well-run. Reviews show online group therapy is feasible and can match face-to-face outcomes, though facilitators must manage energy, norms, and tech. Look for small, stable cohorts with clear rules and practice time.
4) What if my internet is unreliable?
Plan a low-bandwidth fallback: switch off video, use phone audio, or have a backup phone session with a structured agenda. Ask about captions and transcripts if you need them. Bandwidth shouldn’t become a barrier to access or dignity.
5) Are digital self-help tools worth it without a therapist?
Guided programs typically outperform unguided ones. If you start unguided, pair the tool with brief accountability (friend, coach, or check-ins) and track your outcomes so you can switch to guided care if progress stalls.
6) How often should I meet if I’m doing hybrid?
Begin weekly for momentum. After 6–8 weeks, consider alternating online and in-person or tapering to biweekly if your outcomes are improving. Use switch triggers (e.g., symptom scores, missed sessions) to adjust cadence.
7) What about privacy at home?
Headphones, a closed door, white-noise apps, and disabling smart speakers go a long way. Don’t record sessions without explicit agreement. Confirm your provider’s data retention policies and platforms.
8) Can I do exposure or skills practice online?
Absolutely—many exercises translate well with screen-sharing, guided practice, and between-session tasks. For complex or safety-sensitive exposures, in-person can help; a hybrid plan lets you rehearse online and perform live with support.
9) Does teletherapy help underserved or rural communities?
It can—by cutting travel time and stigma and widening provider choice. But equity requires more than access: language support, disability accommodations, device/bandwidth solutions, and outcome monitoring. Global strategies emphasize building this infrastructure.
10) How do I measure whether it’s working?
Use PHQ-9 and GAD-7 every 2–4 weeks, add one functional KPI, and review monthly. If scores plateau or worsen, change something: cadence, modality, or approach. Systems like NHS Talking Therapies do this routinely; you can mirror that at home.
11) Is the therapeutic bond weaker online?
Not necessarily. With good teletherapy skills, alliance and outcomes in online care can match in-person. Eye-level camera, strong audio, and deliberate relational behaviors preserve presence.
12) When should I avoid online care?
If you’re in acute crisis (active suicidal intent, severe withdrawal, psychosis) or cannot secure privacy, seek in-person or emergency care first. Online can re-enter the plan after stabilization with explicit crisis protocols.
Conclusion
“Online vs. in-person” isn’t a contest; it’s a toolkit. Online care broadens access and maintains outcomes for many common needs, while in-person care anchors safety, complexity, and certain experiential work. The most durable plans are hybrid: they start where you can get traction fast, layer in the depth you need, and use simple data to decide what to adjust. Protect privacy and safety up front, choose evidence-based tools, and join groups designed for cohesion—not just convenience. Above all, let your goals lead. When your symptom trends and real-life functioning guide modality switches, you can preserve momentum, reduce relapse risk, and spend less time second-guessing the format and more time living the gains.
CTA: Pick one metric (PHQ-9 or GAD-7), one cadence (weekly), and one switch rule—then book your next session in whichever format you’re most likely to keep.
References
- Psychiatric Treatment Conducted via Telemedicine Versus In-Person: A Systematic Review and Meta-Analysis, JMIR Mental Health, 2023. JMIR Mental Health
- Effectiveness of Telehealth Versus In-Person Care During the COVID-19 Pandemic: Systematic Review, BMC Health Services Research, 2024. PMC
- The Association Between Quality of Therapeutic Alliance and Treatment Outcomes in Teletherapy: A Systematic Review and Meta-Analysis, Clinical Psychology Review, 2024. PubMed
- Therapeutic Alliance and Clinical Outcomes in Teletherapy and In-Person Psychotherapy: A Noninferiority Study, Psychotherapy Research, 2024. Taylor & Francis Online
- Online Group Psychotherapy: A Systematic Review, Frontiers in Psychiatry, 2024. PMC
- APA Guidelines for the Practice of Telepsychology (Revisions), American Psychological Association, updated 2023. American Psychological Association
- New Telepsychiatry Resources for 2023, American Psychiatric Association & American Telemedicine Association, 2023. American Psychiatric Association
- Global Strategy on Digital Health 2020–2025, World Health Organization, 2021. World Health Organization
- The NHS Talking Therapies for Anxiety and Depression Manual (Version 7), NHS England/Royal College of Psychiatrists, 2023. www.rcpsych.ac.uk
- Effectiveness of Videoconference-Delivered Cognitive Behavioral Therapy: Systematic and Meta-Analytic Review, Journal of Medical Internet Research, 2021. JMIR
- Internet-Based CBT for Depression: Individual Patient Data Network Meta-analysis, JAMA Psychiatry, 2021. JAMA Network
- Social Presence: Conceptualization and Measurement, Frontiers in Psychology, 2021. PMC