Good sleep is not just “rest”—it’s training you don’t have to sweat for. Sleep habit tracking means consistently monitoring the timing, duration, and quality of your sleep so you can adjust training, recovery, and daily routines with evidence instead of vibes. Done well, it helps you hit personal records, feel sharper, and stay healthier with fewer injuries. In plain terms: track your sleep, connect the dots, and you’ll train smarter.
Quick answer: Adults generally need at least 7 hours of sleep for health; athletes often need more. Tracking core metrics—duration, regularity, latency, efficiency, HRV—helps you tailor training load, nutrition, and wind-down habits for better performance.
This guide is educational and not medical advice. If you suspect a sleep disorder (e.g., loud snoring, pauses in breathing, persistent insomnia, excessive sleepiness), talk to a qualified clinician.
1. Set Baseline Targets for the Metrics That Matter
The fastest way to get value from sleep tracking is to lock in a small set of clear targets: duration, regularity, sleep latency (how fast you fall asleep), and sleep efficiency (how much of your time in bed you actually sleep). Adults should aim for at least 7 hours nightly; many active people need 7–9+. Strive to fall asleep in about 10–20 minutes and keep sleep efficiency near 85–90%. Track these for two weeks before changing your training: a baseline helps you see if bad workouts come from sleep debt or from the plan. Finally, step on the scale of consistency: similar sleep/wake times (regularity) stabilize circadian biology, which supports recovery and energy.
1.1 Why it matters
- Duration: Less than 7 hours on average is linked to higher cardiometabolic risk and impaired performance.
- Latency: <10 minutes may signal sleep debt; >20–30 minutes flags insomnia risk or poor sleep hygiene.
- Efficiency: Below ~85% suggests fragmented sleep; CBT-I protocols use 85% as a key threshold.
- Regularity: Stable timing reduces circadian strain and associates with better health outcomes.
1.2 Mini-checklist
- Log 14 nights of duration, bedtime/wake-time, latency, and overnight awakenings.
- Compute efficiency = (total sleep time ÷ time in bed) × 100.
- Flag any week with >2 nights under 7 hours or efficiency <85% for course correction.
Bottom line: The fewer metrics you chase, the faster you’ll act on them—and the better your training will feel.
2. Make Sleep Regularity a Performance Habit (Not Just Total Hours)
Regularity means going to bed and waking up at similar times daily. Two athletes can both average 7.5 hours—yet the one with consistent timing usually feels and performs better. The Sleep Regularity Index (SRI) captures day-to-day stability; lower SRI (more irregular) is linked to worse cardiometabolic markers and, in large cohorts, higher mortality risk. For practical purposes, keep your wake time within ±30 minutes across the week and anchor your light exposure: bright light in the morning, dimmer light at night. If evenings vary due to work, protect the wake time and use brief afternoon naps (see §7). Nature
2.1 Numbers & guardrails
- SRI typical range: ~30–95; aim higher over time. Frontiers
- Morning light: 5–20 minutes outdoors helps set the clock; evening bright light, especially blue-enriched, can delay melatonin (magnitude varies by brightness/duration/content). PubMed
2.2 Common mistakes
- Weekend drift (“social jet lag”) undoing weekday gains.
- Chasing deep sleep percentages instead of regularity.
- Bright screens late—but note that engagement and overall light level matter as much as color.
Bottom line: Protecting consistent timing is the simplest high-impact sleep upgrade you can make for training.
3. Connect Sleep to Training Load: Fewer Injuries, Better Outputs
Sleep tracking is not about pretty charts; it’s about performance and availability. Evidence shows that more sleep (or extending sleep) can improve sport-specific outputs, and insufficient sleep correlates with higher injury risk in youth athletes. In the well-known Stanford basketball study, players targeted up to 10 hours in bed and improved sprint times and shooting accuracy; meanwhile, adolescent athletes sleeping <8 hours were 1.7× more likely to be injured. In elite sport, a 2021 consensus highlights frequent short sleep and fragmentation in athletes and discourages building training on top of sleep restriction. Use this: if your sleep duration or efficiency drops for 2–3 nights, scale back intensity until you rebound.
3.1 How to do it
- Tag each training log with prior-night sleep duration/efficiency.
- Look for patterns: poor interval days after <7 h or efficiency <85%.
- Pre-meet plan: prioritize earlier wind-downs and a stable wake time 7–10 days out.
3.2 Mini case
- After bumping weekly mileage by 15%, you log three nights at 6:15–6:45 sleep and <80% efficiency. Your next two workouts feel flat. You deload 48–72 hours, add a 20-minute nap, and return to baseline paces.
Bottom line: Sleep is a training variable—plan it like volume and intensity.
4. Use Wearable Data Wisely: Trust Trends Over Stages
Wearables make tracking easy, but they’re not diagnostic tools. The American Academy of Sleep Medicine states consumer sleep tech can inform habits yet isn’t cleared to diagnose/treat disorders. Accuracy for total sleep time and wake after sleep onset is generally decent; sleep staging (light/deep/REM) is weaker and varies across devices and updates. For example, a 2024 study on Oura Gen3 found staging accuracy ranging roughly 76–91% by stage, while a 2025 analysis comparing ring trackers showed ~53% overall stage accuracy for some devices—fine for trends, not medical decisions. With WHOOP, peer-reviewed work supports acceptable accuracy for sleep duration and cardiac variables; still, use it to guide behavior, not to self-diagnose apnea.
4.1 Tools/Examples
- Good to track: total sleep time, time in bed, sleep/wake timing, awakenings, HR/HRV trends.
- Handle with care: nightly deep/REM percentages; don’t obsess over a single night’s score.
- Golden rule: Believe patterns over points—3–7-day rolling averages beat one-night swings.
4.2 Mini-checklist
- Pick one device/app and stick to it for at least a 4-week block.
- Export weekly summaries; annotate with training load and caffeine/alcohol notes.
- If sleep scores crash without cause (and you feel fine), power-cycle the device, then revert to how you feel plus basic metrics.
Bottom line: Wearables are great coaches for habits, not doctors for diagnoses.
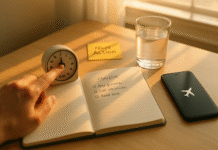
5. Build a Personal Sleep Scorecard You’ll Actually Use
A simple scorecard makes your data actionable. Track bedtime, wake time, time in bed, total sleep time, latency, awakenings, efficiency, perceived energy (1–5), and next-day training quality. Add two modifiers: caffeine after 2 p.m. (Y/N) and alcohol (Y/N). Rate soreness and mood. Review weekly: if sleep efficiency dips <85% or your average latency creeps >20 minutes, adjust wind-down, training load, or stimulants. If you prefer analog, a pen-and-paper sleep diary works; digital types can sync Apple Health, Google Fit, Garmin, Oura, or WHOOP and export CSVs. (If insomnia persists >3 months, ask about CBT-I, which uses sleep efficiency targets to reset patterns.) Sleep Foundation
5.1 Quick template (copy this into notes/spreadsheet)
- Bed / Wake (hh:mm), TIB (h:mm), TST (h:mm), Latency (min), Awakenings (#), Efficiency (%), Energy (1–5), Training Quality (1–5), Caffeine after 14:00, Alcohol, Notes.
5.2 Weekly review questions
- What preceded my best workouts?
- Do late nights cluster before hard training days?
- Which single change (earlier dinner, earlier light-out) correlates with better efficiency?
Bottom line: A scorecard turns tracking into decisions in minutes.
6. Track the “Big Two” Sleep Disruptors: Caffeine and Light
Two things sabotage sleep the most: stimulating your biology (caffeine) and confusing your body clock (late bright light). The FDA notes up to 400 mg/day caffeine is generally safe for most adults, but the half-life varies widely (roughly 2–12 hours), so a 3 p.m. latte can still be in your system at 10 p.m. For light, blue-rich light at night suppresses melatonin and can delay sleep, though the impact depends on brightness, duration, and content engagement—darkening your environment and winding down still wins. Track your late-day caffeine and evening light exposure alongside sleep efficiency and latency to see cause-effect.
6.1 Practical guardrails
- Caffeine curfew: stop 6–8 hours before bedtime (earlier if sensitive).
- Evening light: dim household lights; enable warm/night modes; switch to low-engagement tasks (paper book, stretch).
- Morning light: get outside within an hour of waking.
6.2 Mini numeric example
- Espresso at 2 p.m. (~75 mg): with a 5-hour half-life, ~37 mg remains at 7 p.m., ~18 mg at midnight—enough to matter for some sleepers.
Bottom line: Reducing late stimulants and bright light can shave minutes off latency and bump efficiency without changing training at all.
7. Use Strategic Naps to Protect Performance (Without Ruining Night Sleep)
Naps are a legitimate tool when training load spikes or nights run short. Meta-analyses and lab studies show daytime naps (especially 20–30 minutes, or a full ~90-minute cycle) can improve reaction time, sprint ability, and vigilance—classic fitness carryovers. The famous “NASA nap” of ~26 minutes increased alertness by up to 54% and performance by 34% in pilots. For athletes, schedule naps 6–8 hours after wake time, keep them before 3–4 p.m., and leave 30 minutes between waking and hard training to shake off inertia. British Journal of Sports Medicine
7.1 How to do it
- Short nap (20–30 min): quick alertness boost; avoid deep sleep.
- Long nap (~90 min): full cycle if sleep debt is large; use sparingly if it delays bedtime.
- Pre-event: if travel wrecked sleep, a 20-minute nap 3–4 hours before start time can steady performance. PMC
7.2 Common mistakes
- Napping too late (hurts sleep pressure at night).
- No buffer before workouts (grogginess).
- Assuming naps “replace” night sleep—they mitigate, not cure debt.
Bottom line: Track naps as part of your plan; used right, they’re free performance.
8. Fuel and Wind-Down for Overnight Recovery
What you do in the last 2–3 hours before bed shows up in your sleep log. Heavy meals and alcohol close to bedtime fragment sleep and hurt efficiency; light, balanced dinners earlier help. If strength is a priority, research shows pre-sleep protein (20–40 g casein/slow-digesting) can increase overnight muscle protein synthesis without harming sleep—trial it and track how you feel. Pair this with a calm wind-down: dim lights, 5–10 minutes of mobility or breathing, and cool bedroom (~17–19°C / 63–66°F). Track latency and efficiency to see what sticks.
8.1 Mini-checklist
- 2–3 h pre-bed: finish dinner; cap alcohol.
- 60 min pre-bed: screens low/warmer; light tidy/stretch/read.
- Lights out: all lights off/blocked; room cool; fan or white noise if needed.
8.2 Numeric example
- Over two weeks, you add 30 g casein 30–60 minutes pre-bed and shift dinner earlier by 45 minutes. Your efficiency average climbs from 82% → 88% and morning RPE drops by 1 point—track-backed wins.
Bottom line: Your evening routine is a lever you can pull every day; let sleep data verify the impact.
9. Monitor HRV and Resting Heart Rate to Tune Readiness (With Context)
Heart rate variability (HRV)—often reported as RMSSD—and resting heart rate (RHR) during sleep can reflect how recovered your nervous system is. Higher HRV (for you) and lower RHR usually indicate better readiness; sustained drops in HRV with elevated RHR suggest stress, sickness, or overload. Reviews in athletes support HRV as useful for monitoring training status and recovery, but individual baselines matter far more than population “norms.” Track nightly values and watch the 7-day trend; adjust intensity if HRV slumps for 3–4 days alongside poor sleep.
9.1 Tools/Examples
- Use your device’s night HRV; prefer RMSSD due to reliability. SpringerOpen
- Expect HRV to decline with age; compare you to you. (Population ranges vary widely.) PMC
9.2 Mini-checklist
- Track HRV + RHR nightly; review with sleep efficiency.
- If HRV ↓ and RHR ↑ ≥3 days (and you feel off), cut intensity by 20–40%, bias volume to easy, and prioritize earlier bedtime.
Bottom line: HRV is a helpful “second opinion” when combined with sleep duration/efficiency and how you actually feel.
10. Know When to Escalate: From Tracking to Clinical Help
Sleep tracking is powerful—but it has limits. If your data show chronic short sleep, extreme sleepiness, very low efficiency, or signs of a disorder, escalate. Red flags include: loud snoring/gasping, witnessed apneas, unrefreshing sleep despite long time in bed, or insomnia persisting >3 months. Consumer devices aren’t diagnostic; AASM guidance is clear on this. A clinician may use formal tools like polysomnography or multiple sleep latency tests (normal mean sleep latency is typically 10–20 minutes) to evaluate disorders. If insomnia is the issue, ask about CBT-I, which uses sleep efficiency thresholds (often 85%) to reset timing and consolidate sleep. Keep sharing your sleep log—it accelerates care.
10.1 Mini-checklist for seeking help
- Symptoms persist >3 months or impair life/training.
- Partner notes snoring or pauses; you wake choking/gasping.
- Epworth Sleepiness Scale ≥10 and/or you doze unintentionally.
Bottom line: Tracking gets you 80% there; the last 20% may require professional evaluation and treatment.
FAQs
1) What is “sleep habit tracking,” exactly?
It’s the consistent monitoring of sleep timing, duration, and quality—usually with a wearable and/or a sleep diary—then acting on trends. Core metrics include total sleep time, latency (time to fall asleep), efficiency (percent of time in bed spent asleep), regularity (consistency of timing), and sometimes HRV. The goal is not perfect numbers but better training decisions: when to push, when to pull back, and which routines actually help.
2) How many hours should active adults aim for?
Most adults benefit from at least 7 hours; athletes or people in heavy training often do better with 7–9+ hours, especially before key sessions and competitions. Short sleep increases cardiometabolic risks and can blunt performance. If 7+ hours feels impossible right now, start by adding 15–30 minutes and standardizing wake time.
3) Do I need to worry about deep vs. REM percentages every night?
Not really. Night-to-night sleep staging is the noisiest part of consumer devices. Focus on total sleep, regularity, and efficiency first. Staging trends can be interesting, but they’re not a reliable basis for medical decisions. If you’re sleeping enough, at consistent times, and feeling good, you’re winning.
4) What’s a “good” sleep efficiency?
In clinical insomnia care and sleep restriction therapy, ~85% is a key threshold: below that suggests fragmented sleep, while 85–90% reflects consolidated sleep. If you’re persistently <85%, look for causes (late caffeine, alcohol, stress, pain, pets/kids, room temperature) and consider CBT-I strategies. Stanford Health Care
5) How late is too late for caffeine?
Caffeine’s half-life ranges roughly 2–12 hours, with an average near 5 hours and big individual differences. As a rule of thumb, cut caffeine 6–8 hours before bed. If you’re sensitive, move your last cup even earlier. Track latency/efficiency on days you break the rule—you’ll see the effect. PMC
6) Does blue light really ruin sleep?
Bright light at night, blue-enriched or otherwise, suppresses melatonin and can delay sleep—especially with prolonged exposure. That said, total brightness and what you’re doing on the device matter too; doom-scrolling is stimulating regardless of color. Dim the environment, shift to calmer tasks, and wind down predictably. WIRED
7) Can naps replace a bad night’s sleep?
Naps help but don’t fully replace night sleep. Short 20–30 minute naps improve alertness with minimal grogginess; longer ~90-minute naps can help if debt is large but may push bedtime later. The well-known ~26-minute NASA nap boosted alertness and performance meaningfully in pilots.
8) Is HRV a must-track metric?
It’s useful—especially RMSSD—as a personal trend for stress/recovery. Combine it with sleep duration/efficiency and subjective feel. Don’t chase population “normals” (they vary widely); compare you vs. you across weeks. If HRV dips for days alongside poor sleep and higher RHR, consider a lighter block. PMC
9) I’m training hard but always tired. Should I just sleep more?
First, audit sleep regularity, efficiency, and sleep debt. If they’re off, fix them. If you’re doing most things right but still wake unrefreshed, screen for sleep apnea or insomnia, both common and treatable. Consumer wearables aren’t diagnostic—talk to a clinician about appropriate testing (PSG, MSLT).
10) Does pre-sleep protein help recovery?
For lifters and team-sport athletes, 20–40 g of slow-digesting protein (e.g., casein) before bed can increase overnight muscle protein synthesis and support recovery, without harming sleep in most people. Try it for 2–3 weeks and track how you feel and perform.
Conclusion
If training is your stress, sleep is your recovery system. Sleep habit tracking turns “I guess I slept OK” into a feedback loop you can actually coach: set a few clear targets (≥7 hours, consistent timing, 10–20 min latency, 85–90% efficiency), reduce late stimulants and light, and correlate sleep with training outputs and readiness (HRV/RHR). Use wearables for trends—not medical calls—and keep a simple scorecard so the signal isn’t buried in noise. When patterns point to chronic issues, escalate to clinical care; effective tools like CBT-I and formal testing can resolve what data alone can’t.
The playbook is simple: protect regularity, bank enough hours, fine-tune the wind-down, and use naps strategically. Start with a two-week baseline, make one change at a time, and let your sleep and workout logs tell you what works.
Ready to upgrade your training? Tonight, set a consistent lights-out and track it for 14 days—then build from there.
References
- FastStats: Sleep in Adults, Centers for Disease Control and Prevention (May 15, 2024). CDC
- Prevalence of Healthy Sleep Duration among Adults—United States, 2014, CDC / MMWR (Feb 19, 2016). CDC
- National Sleep Foundation’s Sleep Time Duration Recommendations, Sleep Health (2015). https://www.sleephealthjournal.org/article/S2352-7218(15)00015-7/fulltext Sleep Health Journal
- The Effects of Sleep Extension on the Athletic Performance of Collegiate Basketball Players, SLEEP (2011). PMC
- Chronic Lack of Sleep Is Associated With Increased Sports Injuries in Adolescent Athletes, Journal of Pediatric Orthopaedics (2014). PubMed
- Sleep and the Athlete: 2021 Expert Consensus Recommendations, British Journal of Sports Medicine (2021). British Journal of Sports Medicine
- Consumer Sleep Technology: An American Academy of Sleep Medicine Position Statement, Journal of Clinical Sleep Medicine (2018). PMC
- Validity and Reliability of the Oura Ring Generation 3 Compared to Polysomnography, Sleep Medicine (2024). PubMed
- Performance of Wearable Finger Ring Trackers for Diagnostic Sleep Staging, npj Digital Medicine (2025). PMC
- Recommended Protocols for the Multiple Sleep Latency Test, Journal of Clinical Sleep Medicine (2021). JCSM
- Measuring Sleep Efficiency: What Should the Denominator Be?, Journal of Clinical Sleep Medicine (2016). PMC
- Sleep Latency—What It Is and Why It Matters, Sleep Foundation (updated 2025). Sleep Foundation
- Spilling the Beans: How Much Caffeine is Too Much?, U.S. FDA (Aug 28, 2024). U.S. Food and Drug Administration
- How Long Does It Take for Caffeine to Wear Off?, Sleep Foundation (Jul 16, 2025). Sleep Foundation
- Blue Light Has a Dark Side, Harvard Health Publishing (updated Jul 24, 2024). Harvard Health
- NASA Nap: How a 26-Minute Nap Improves Performance, Sleep Foundation (Oct 27, 2023). Sleep Foundation
- Pre-Sleep Protein Ingestion to Improve Skeletal Muscle Adaptive Response to Exercise, Frontiers in Physiology (2016). PMC
- Acute Sleep Deprivation Decreases Muscle Protein Synthesis, Physiological Reports (2021). PMC
- The Importance of Sleep Regularity: A Consensus Statement, Sleep Health (2023). https://www.sleephealthjournal.org/article/S2352-7218(23)00166-3/fulltext Sleep Health Journal
- Sleep Regularity Is a Stronger Predictor of Mortality Risk Than Sleep Duration, Sleep (2023). PMC