Getting relaxed enough to drift off isn’t just “mind over mattress.” It’s biology. The science behind relaxation and sleep explains why some nights feel effortless and others don’t. In this guide, you’ll learn nine proven pillars that tilt your body toward calm, shorten the time it takes to fall asleep, and improve the quality of the sleep you get. This article is educational and not a substitute for medical advice or care; if insomnia persists, speak with a qualified clinician.
Quick answer: Relaxation and sleep arise when your autonomic nervous system shifts toward parasympathetic (“rest-and-digest”) activity while two sleep systems—circadian timing and homeostatic sleep pressure—align, supported by light, temperature, breathing, neurotransmitters, and behavior. The nine pillars below show where to focus.
1. Autonomic Balance & Vagal Tone: The Switch Into “Rest-and-Digest”
Relaxation begins when your autonomic nervous system rebalances toward parasympathetic dominance; this calms heart rate, slows breathing, and quiets threat detection—conditions that make sleep possible. A practical way to trigger this switch is through slow, nasal, diaphragmatic breathing at ~6 breaths per minute (about 0.1 Hz), which amplifies respiratory sinus arrhythmia and heart rate variability (HRV), a non-invasive biomarker of vagal activity. Studies and reviews show that slow breathing and related practices improve HRV, lower perceived stress and cortisol, and support emotional regulation—an ideal on-ramp to sleep. HRV isn’t just a number on a wearable; it reflects your body’s capacity to flexibly shift out of “fight-or-flight” and into recovery. Breathing gives you a handle on this physiology in minutes, not months.
1.1 Why it matters
- HRV as a proxy: Higher HRV generally indicates stronger vagal (parasympathetic) influence and better stress resilience, which correlates with easier sleep initiation.
- Resonance breathing: Around six breaths per minute typically maximizes HRV by syncing baroreflex, breathing, and heart rhythms.
- Immediate effects: Even brief slow-breathing bouts reduce tension and perceived stress, with measurable autonomic changes. MDPI
1.2 How to do it (mini-checklist)
- Sit or lie down; close your mouth; inhale through your nose into the belly for ~5 seconds, exhale for ~5 seconds.
- Continue for 5–10 minutes, keeping breaths quiet and effortless.
- If you use a wearable, watch HRV or breathing rate settle; if not, use how your body feels (warmth, jaw unclenching) as feedback.
- Layer in progressive muscle relaxation (tense 5–7 muscle groups for ~5 seconds, then release) if you carry a lot of bodily tension.
- Practice earlier in the evening first; keep a short 3–5 minute “top-up” in bed.
Synthesis: You can’t force sleep, but you can invite it. Deliberate slow breathing and gentle muscle release reliably tip your autonomic balance toward rest, making all other sleep levers more effective.
2. The HPA Axis & Cortisol: Aligning Stress Hormones With Night
Your hypothalamic-pituitary-adrenal (HPA) axis sets daily cortisol rhythms that wake you in the morning and should quiet down by night. When cortisol stays high in the evening—because of stress, late caffeine, intense late-night exercise, or irregular schedules—sleep onset can drag and awakenings become more likely. Research shows cortisol output is shaped by circadian timing and the sleep–wake cycle; chronic insomnia is associated with moderately elevated 24-hour cortisol, indicating persistent HPA activation. Night-shift work and irregular routines can further blunt or shift cortisol rhythms, compounding sleep problems.
2.1 Numbers & guardrails
- Normal pattern: Cortisol is typically lowest near midnight, rises before dawn (the “cortisol awakening response”), then tapers across the day.
- Insomnia link: Meta-analyses note moderately increased cortisol in chronic insomnia.
- Shift work: Night shifts disrupt cortisol’s circadian rhythm, with downstream health risks. PMC
2.2 Down-regulating by evening (tips)
- Buffer zone: Aim for a 60–90-minute pre-bed wind-down without work email, doom-scrolling, or heated conversations.
- Gentle inputs: Use low-arousal activities—stretching, reading fiction, guided breathing—to avoid stress spikes.
- Predictability: Keep consistent sleep/wake times (±30–60 minutes), including weekends, to stabilize HPA rhythms.
- Light timing: Get bright outdoor light soon after waking; keep evenings dim (see Pillar 3).
Synthesis: Sleep improves when cortisol follows its natural day-night arc. Protect evenings from stimulation and keep mornings bright to let the HPA axis do its job—high by day, low at night.
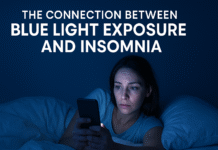
3. Circadian Timing & Melatonin: Light Is the Steering Wheel
Your circadian pacemaker (the suprachiasmatic nucleus, SCN) times melatonin release and orchestrates the daily rise and fall of sleep drive, body temperature, and alertness. Light—especially bright, blue-enriched light—suppresses melatonin and shifts clock timing; darkness allows melatonin to rise and signals the body to prepare for sleep. Controlled studies show blue-enriched morning light drops melatonin faster and boosts alertness; at night, short-wavelength light is disproportionately melatonin-suppressing compared with longer wavelengths. Metrics linking light spectrum, intensity, and timing to melatonin suppression continue to evolve, but the practical pattern is clear: brightness and timing matter most.
3.1 Why it matters (as of August 2025)
- Blue-enriched effects: Blue-enriched (∼6,500 K) morning light accelerates melatonin decline and improves subjective alertness.
- Evening exposure: Experimental work shows blue light can suppress melatonin within an hour and keep it suppressed into the night.
- Measurement progress: Recent reviews formalize metrics to predict melatonin suppression from spectrum and intensity.
3.2 How to do it (evening & morning)
- Morning: Get 20–30 minutes of outdoor light shortly after waking, even on cloudy days.
- Evening: From ~2 hours before bed, dim overheads; favor warm-tone task lights; reduce screen brightness or use “night modes.”
- If screens are necessary: Keep content non-activating; lower brightness; consider blue-blocking strategies—benefit varies by person and setting.
Synthesis: Use bright, preferably outdoor light to anchor your clock by day, and dial down light exposure at night so melatonin can rise on schedule. That simple rhythm makes every other pillar more effective. PMC
4. Homeostatic Sleep Pressure & Adenosine: Build It Up, Don’t Block It
The longer you’ve been awake, the stronger your drive to sleep—thanks in large part to adenosine, a neuromodulator that accumulates during wakefulness and promotes sleep via A1 and A2A receptors. Caffeine makes you feel alert because it blocks those receptors; timing and dose matter. Systematic reviews show caffeine can reduce total sleep time (~45 minutes on average), lower sleep efficiency, and delay sleep onset—even when taken hours before bed. After days of short sleep, adenosine receptors upregulate, which can intensify sleepiness until you repay the debt.
4.1 Numbers & guardrails
- Mechanism: Adenosine is a homeostatic sleep factor; caffeine antagonizes A1/A2A receptors to reduce sleepiness. ScienceDirect
- Impact on sleep: Meta-analyses note ~45 minutes less total sleep and increased wake after sleep onset with caffeine.
- Timing & dose: Newer work suggests 400 mg can impair sleep even when consumed up to 12 hours pre-bed; lower doses are safer closer to bedtime. Individual sensitivity varies.
4.2 Practical playbook
- Cutoff: Many people sleep better stopping caffeine by early afternoon; sensitive sleepers may need a noon cutoff.
- Dose: Track total daily intake (coffee, tea, energy drinks, pre-workouts, dark chocolate).
- Debt repayment: If you’ve slept poorly, a short early afternoon nap (10–20 minutes) can help without harming night sleep; avoid late naps that dissipate adenosine too close to bedtime.
Synthesis: Don’t fight biology. Let adenosine accumulate and avoid blocking it late in the day—sleep pressure is one of your strongest allies for effortless sleep.
5. Inhibitory Tone (GABA) & Thalamocortical Rhythms: Quieting the Brain
Falling asleep isn’t just “getting tired”; it’s a coordinated shift in neural networks. GABA—the brain’s principal inhibitory neurotransmitter—rises in influence at sleep onset, helping dampen cortical activity. In the thalamus and cortex, GABAergic circuits produce sleep spindles and slow-wave activity that stabilize non-REM sleep and support memory processes. Disturbances in the GABA–glutamate balance are linked to insomnia and fragmented sleep. While sedative-hypnotic drugs act on GABA_A receptors, non-drug approaches (relaxation, breathing, CBT-I) can help normalize inhibitory tone without side effects.
5.1 Why it matters
- GABA & sleep: Reviews highlight GABA’s central role in initiating and maintaining sleep; dysregulation is implicated in insomnia. Cell
- Thalamocortical rhythms: Sleep spindles and slow waves rely on GABAergic mechanisms; altering receptor subunits changes NREM delta power.
5.2 Tools & examples
- Wind-down inputs: Progressive muscle relaxation, slow breathing, and mindfulness practices reduce cortical arousal—supporting GABAergic quieting. (See Pillar 1 and Pillar 8.)
- Content diet: Avoid cognitively activating tasks (intense work, competitive gaming) late at night; cognitive load can counter inhibitory tone.
- Mini case: A ruminative mind at bedtime often reflects high cortical excitation—adding 10 minutes of slow breathing followed by a scripted body scan can reduce time-to-sleep within a week for many sleepers.
Synthesis: Sleep takes hold when inhibitory networks win. Give your brain permission to idle by lowering cognitive arousal and tapping practices that favor GABA-guided rhythms.
6. Thermoregulation: Warm Up, Then Cool Down
Sleep starts more readily as core body temperature (CBT) naturally declines in the evening. The body facilitates this by increasing heat loss through distal skin (hands/feet), which raises the distal-to-proximal temperature gradient. Strategically using heat before bed—then letting the body cool—can shorten sleep onset and deepen early-night sleep. A landmark meta-analysis shows that a warm bath or shower (∼40–42.5 °C) taken 1–2 hours before bed for as little as 10 minutes reduces sleep onset latency; other experiments highlight how cutaneous warming around the eyes or feet promotes heat loss and faster sleep onset. Meanwhile, an excessively warm bedroom blocks heat dissipation and fragments sleep.
6.1 Numbers & guardrails
- “Warm bath effect”: 40–42.5 °C water, 1–2 hours pre-bed, can meaningfully shorten time-to-sleep and improve efficiency.
- CBT dynamics: Sleep onset occurs on the downslope of CBT; a <1 °C shift can matter.
- Skin warming evidence: Warming periocular skin enhances distal heat loss and shortens sleep onset in people with sleep difficulty. Frontiers
6.2 Practical setup (mini-checklist)
- Bath or shower: 10–20 minutes in warm (not scalding) water 60–120 minutes before bed.
- Bedroom climate: Keep the room cool and well-ventilated; breathable bedding helps maintain a comfortable “bed microclimate.”
- Hands & feet: Warm socks in a cool room can accelerate heat loss from the core by promoting distal vasodilation.
- Post-workout: Allow enough cooldown after evening exercise so CBT can fall again before bedtime.
Synthesis: Encourage heat out of the core before bed and avoid trapping it overnight. Warm to trigger vasodilation, then cool to ride CBT’s natural decline into deeper sleep. BioMed Central
7. Sleep Architecture, Memory & Brain Cleansing: Why Deep Sleep Feels Restorative
Sleep isn’t uniform. Non-REM stages (especially slow-wave sleep) stabilize physiology and support memory consolidation, while REM fine-tunes emotional processing. On the cellular side, sleep seems to enhance clearance of metabolic by-products via the glymphatic system, with classic experiments showing increased convective exchange of cerebrospinal and interstitial fluid during sleep. Newer human imaging and reviews suggest that poor sleep quality can weaken glymphatic-related transport and correlate with memory decline. While scientists continue to refine the story in humans, the practical takeaway is consistent: protect deep sleep—particularly early in the night—because it carries outsized restorative benefits.
7.1 Why it matters
- Metabolite clearance: Foundational work demonstrated ~60% expansion of interstitial space and enhanced clearance during sleep (rodent), a mechanistic rationale for sleep’s restorative feel.
- Human signals: Emerging imaging and modeling studies link better sleep with stronger glymphatic transport; poor sleep shows reductions. Nature
- Memory consolidation: Meta-analyses and mechanistic reviews implicate NREM slow waves and spindles in stabilizing memories. PMC
7.2 Protecting architecture (tips)
- Front-load recovery: Prioritize a consistent bedtime; early-night slow-wave sleep is most sensitive to heat, alcohol, and caffeine.
- Stabilize inputs: Keep the room dark and quiet; minimize awakenings that fragment stage transitions.
- Allow oscillations: Practices that reduce arousal (breathing, relaxation) help your brain “hand off” to deeper stages smoothly.
Synthesis: You don’t need to hack every stage—just protect the conditions that let deep NREM unfold. The brain will handle memory and housekeeping if you give it the chance. HKU – Department of Psychology
8. Cognitive Arousal & CBT-I: Re-training the Brain for Sleep
For many, the obstacle isn’t biology—it’s a learned pattern of wakefulness in bed. Cognitive Behavioral Therapy for Insomnia (CBT-I) targets this by reducing presleep worry, restoring a strong bed-sleep association, and consolidating sleep through stimulus control and sleep restriction. Authoritative guidelines recommend CBT-I as first-line treatment for chronic insomnia in adults. Component analyses consistently show that stimulus control and sleep restriction are especially effective, while relaxation training is useful but should be combined with other components.
8.1 What works (and why)
- Guideline consensus: AASM clinical practice guidelines endorse behavioral and psychological treatments, with CBT-I first-line.
- Power components: Network/meta-analyses highlight stimulus control and sleep restriction as high-impact elements. Wiley Online Library
- Access options: Digital CBT-I can be helpful when trained providers are scarce, though therapist-guided delivery tends to produce larger effects. AASM
8.2 Mini-protocol (sleep efficiency target ≥85%)
- Stimulus control: Go to bed only when sleepy; use the bed for sleep and sex; if awake >20–30 minutes, get up and do a quiet activity under dim light; consistent rise time daily.
- Sleep restriction: Temporarily limit time-in-bed to approximate average sleep time (e.g., 5.5–6.5 hours), then gradually expand as sleep consolidates.
- Cognitive tools: Schedule a “worry window” earlier in the evening; jot down to-dos; practice brief breathing/relaxation before lights out.
Synthesis: When insomnia is learned, it must be unlearned. CBT-I rebuilds your sleep system’s confidence by retraining associations and gently tightening timing until efficient sleep returns.
9. Environment & Behavior: Make the Bedroom Do Half the Work
Even perfect biology can be undone by the wrong environment. Noise as low as typical street levels can fragment sleep; light leaks suppress melatonin; alcohol and late heavy meals alter architecture; mistimed exercise or screens can rev you up. Start by optimizing what you can control: darkness, quiet, cool, and a predictable routine. Evidence-based guidelines for environmental noise recommend keeping outdoor Lnight below ~40 dB and bedroom noise as low as practical; while you can’t soundproof the world, white noise or earplugs often help. On the behavior side, exercise improves sleep quality overall (dose and timing matter), alcohol suppresses REM and fragments sleep later in the night, and late caffeine can meaningfully reduce sleep time.
9.1 Tools & guardrails
- Dark + quiet: Aim for a dark room; for noise, target the lowest levels you can manage—WHO documents recommend outdoor night noise under ~40 dB and very quiet bedrooms for high-quality sleep.
- Exercise: Regular physical activity improves subjective and objective sleep; vigorous sessions are best wrapped ≥4 hours before bedtime if you’re sensitive. Evidence is mixed on very-late workouts—find your threshold.
- Alcohol: Even low to moderate evening alcohol reduces REM and degrades architecture; avoid relying on it as a “sleep aid.” ScienceDirect
- Caffeine: See Pillar 4; a 6–12-hour buffer helps many sleepers.
9.2 Mini-checklist (put it together)
- Blackout curtains or a sleep mask; dim warm-tone lights after sunset.
- Keep the room cool and use breathable bedding; consider a fan for airflow.
- White noise or earplugs if you can’t control ambient sounds.
- Plan the last meal 2–3 hours before bed; go lighter if you’re sensitive to reflux.
- Set a consistent rise time; the bedtime will follow.
Synthesis: Your environment can either fight your physiology or flow with it. Make the bedroom cool, dark, quiet, and predictable—then let biology take it from there.
FAQs
1) What’s the single biggest lever for better sleep tonight?
Dim your environment for two hours before bed and finish with 5–10 minutes of slow, nasal breathing in a cool, quiet bedroom. This combination supports melatonin release, builds parasympathetic tone, and eases the CBT decline that initiates sleep. Many people notice a shorter time-to-sleep the first night and more consistent results within a week.
2) Do I need to avoid screens completely at night?
Brightness and timing matter more than the device itself. Lower screen brightness, use warmer color temperatures, and keep content non-activating. If you must use a screen close to bedtime, minimize intensity and exposure; some find blue-blocking helpful, though effects vary. Better yet, replace screens with low-arousal activities during the last hour. Oxford Academic
3) Is a warm bath before bed really worth it?
Yes. A meta-analysis found that a warm bath or shower (∼40–42.5 °C) taken 1–2 hours pre-bed, even for 10 minutes, can shorten sleep onset and improve efficiency by enhancing heat loss from the core via the hands and feet. If you’re short on time, warming your feet or using a warming eye mask in a cool room can mimic some benefits.
4) How late is “too late” for caffeine?
Sensitivity varies, but evidence shows caffeine can cut total sleep time (~45 minutes) and efficiency hours after ingestion. A safe rule is to stop by early afternoon; highly sensitive sleepers may need a noon cutoff. Higher doses (e.g., ~400 mg) can impair sleep even when taken up to 12 hours before bed. Track your response and adjust.
5) Does alcohol help me fall asleep?
Alcohol can make you drowsy, but it suppresses REM early and fragments sleep later as blood alcohol levels fall—often leading to early-morning awakenings. For restorative sleep, keep alcohol modest and earlier in the evening, and avoid using it as a sleep aid.
6) Which exercise timing is best for sleep?
Regular exercise improves sleep quality. If high-intensity sessions near bedtime keep you wired or hot, finish them at least 4 hours before bed. Many people tolerate light evening activity (stretching, yoga, easy walks) without issue. Experiment to find your personal cutoff.
7) How quiet should my bedroom be?
Quieter is better. Environmental guidelines recommend keeping outdoor night noise under ~40 dB (Lnight), and bedrooms as quiet as reasonably possible. If noise is beyond your control, consider earplugs or a consistent white-noise soundscape to mask variability.
8) Is HRV a reliable way to track relaxation before bed?
It’s useful but not perfect. Higher HRV generally reflects greater parasympathetic activity and relaxation, and slow breathing can raise HRV within minutes. Use it as feedback, not a score to obsess over. How you feel and how easily you fall asleep remain the best guides.
9) What if I’m doing “everything right” and still can’t sleep?
Persistent insomnia often involves conditioned wakefulness. CBT-I—especially stimulus control and sleep restriction—rebuilds your sleep system’s efficiency and reduces presleep worry. If symptoms continue or you suspect another sleep disorder (e.g., sleep apnea), consult a clinician for evaluation. ScienceDirect
10) Does deep sleep actually clean the brain?
Animal studies show increased metabolite clearance during sleep, and human imaging is beginning to align with that story. While the exact magnitude in humans is under active study, protecting deep NREM still pays off for cognition and mood. BioMed Central
Conclusion
Relaxation and sleep aren’t mysteries—they’re processes you can support. Shift your autonomic balance toward parasympathetic calm (Pillar 1), let cortisol fall by evening (Pillar 2), manage light to steer melatonin (Pillar 3), and let adenosine do its job by timing caffeine wisely (Pillar 4). Help your brain quiet with inhibitory tone (Pillar 5), ride the night’s natural temperature curve (Pillar 6), and protect the architecture that stabilizes memory and mental health (Pillar 7). If insomnia has become learned wakefulness, retrain it with CBT-I (Pillar 8). Finally, let your environment do half the work—dark, quiet, cool, and consistent (Pillar 9).
Pick one or two pillars to start tonight—the compounding effect is real. Your next best step: set a consistent rise time, dim the last two hours, and breathe slowly for five minutes in a cool, quiet room before lights out. Sleep will meet you halfway.
CTA: Ready to test the pillars? Choose one change for the next seven nights, log your results, and iterate.
References
- Shaffer F, Meehan ZM. A Practical Guide to Resonance Frequency Assessment for Heart Rate Variability Biofeedback. Frontiers in Neuroscience, 2020. https://www.frontiersin.org/articles/10.3389/fnins.2020.570400/full Frontiers
- Gitler A, et al. Harnessing non-invasive vagal neuromodulation: HRV as a biomarker of autonomic flexibility. Frontiers in Neuroscience (PMC), 2025. PMC
- O’Byrne NA, et al. Sleep and Circadian Regulation of Cortisol: A Short Review. Current Opinion in Endocrine and Metabolic Research (PMC), 2021. PMC
- Dressle RJ, et al. HPA axis activity in patients with chronic insomnia: A meta-analysis. Sleep Medicine Reviews, 2022. ScienceDirect
- Haghayegh S, et al. Before-bedtime passive body heating by warm shower or bath to improve sleep: a systematic review and meta-analysis. Sleep Medicine Reviews, 2019. PubMed
- Harding EC, et al. The Temperature Dependence of Sleep. Frontiers in Neuroscience (PMC), 2019. PMC
- Choi K, et al. Awakening effects of blue-enriched morning light exposure on melatonin and alertness. Scientific Reports, 2019. Nature
- de Toledo LHS, et al. Modeling the influence of nighttime light on melatonin suppression in humans. Current Research in Physiology, 2023. ScienceDirect
- Reichert CF, et al. Adenosine, caffeine, and sleep–wake regulation. Current Opinion in Physiology (PMC), 2022. PMC
- Gardiner CL, et al. The effect of caffeine on subsequent sleep: A systematic review and meta-analysis. Sleep Medicine Reviews, 2023/2025 updates. and PubMedOxford Academic
- Edinger JD, et al. Behavioral and psychological treatments for chronic insomnia disorder in adults: An AASM clinical practice guideline. J Clin Sleep Med (PMC), 2021. https://jcsm.aasm.org/doi/10.5664/jcsm.8986 | PMC
- Hablitz LM, et al. The Glymphatic System: A Novel Component of Fundamental Neurophysiology. Journal of Neuroscience (PMC), 2021. PMC
- Xie L, et al. Sleep Drives Metabolite Clearance from the Adult Brain. Science (PMC), 2013. PMC
- WHO Regional Office for Europe. Environmental Noise Guidelines for the European Region. 2018 (overview pages updated 2022). and Environmental Health PerspectivesWorld Health Organization
- Ichiba T, et al. Periocular skin warming promotes body heat loss and sleep onset. Scientific Reports, 2020. Nature
- Kaczmarski P, et al. Influence of glutamatergic and GABAergic neurotransmission on sleep. Frontiers in Neuroscience, 2023. https://www.frontiersin.org/articles/10.3389/fnins.2023.1213971/full Frontiers
- Leota J, et al. Dose-response relationship between evening exercise and sleep. Nature Communications, 2025. Nature
- Colrain IM, et al. Alcohol and the Sleeping Brain. Alcohol Research: Current Reviews (PMC), 2014; plus newer human data. and PMCPubMed
- A52 Breath Narrative Review – Slow, nasal diaphragmatic breathing, HRV and stress outcomes. 2025. PMC
- Sanchez-Cano A, et al. Comparative Effects of Red and Blue LED Light on Melatonin Levels During Three-Hour Exposure in Healthy Adults. Life (MDPI), 2025. MDPI
- Alnawwar MA, et al. The Effect of Physical Activity on Sleep Quality and Duration. International Journal of Environmental Research and Public Health (PMC), 2023. PMC
- Haghani M, Abbasi S. Blue Light and Digital Screens Revisited. Vision (PMC), 2024/2025. PMC