Empathy in healthcare is the clinician’s ability to understand a patient’s feelings and perspective—and to respond in ways that convey that understanding. Done well, it deepens trust, improves shared decisions, and measurably enhances patient experience. This guide translates empathy into 11 concrete strategies you can use today to create safer care, stronger rapport, and better outcomes. Information here is educational and does not replace medical or legal advice; follow your organization’s policies.
Empathy quick-start (60 seconds): Pause and orient → ask one open question → reflect what you heard in one sentence → name the emotion you see → align on the next step.
1. Lead With Proven Empathy Frameworks (NURSE, SPIKES)
Start by using structured playbooks—like NURSE (Name, Understand, Respect, Support, Explore) and SPIKES for hard news—to make empathy reliable under pressure. These frameworks help you respond to emotion without losing clinical clarity, so you can validate feelings, check understanding, and co-create a plan. In real life, pressure, time limits, and complex emotions make “just be empathic” too vague. A shared language gives teams a repeatable approach that works on the ward, in clinic, and over video. When the news is difficult, SPIKES guides the flow from setting up the conversation to strategizing next steps, while NURSE gives you sentence stems that land. Over time, these tools build your default micro-behaviors—sitting at eye level, naming emotion, short summaries—that patients experience as genuine care. PubMedPMC
1.1 How to do it
- Open with purpose: “I want to understand how this is affecting you.”
- NURSE in 30 seconds: “It sounds like you’re worried (Name). I can understand why—this is a lot (Understand). I respect how carefully you’ve tracked your labs (Respect). We’ll support you through each step (Support). Could you share what concerns you most right now? (Explore).”
- SPIKES for serious news: set up → gauge perception → invite → give knowledge → acknowledge emotion → summarize/plan.
1.2 Mini case
A resident must discuss progression on CT. Using SPIKES, she confirms what the patient knows, asks permission to share, delivers news in plain language, pauses for emotion, then uses NURSE to respond. The visit ends with a simple plan and a follow-up call, leaving the patient informed and held.
Synthesis: Frameworks don’t make you scripted; they give you a spine so your warmth and clarity can show up—especially when stakes are high. Comagine Health
2. Listen Deeply—and Close the Loop With Teach-Back
Empathy begins with listening that patients can feel. Start each encounter with one broad question (“What’s most important to cover today?”), listen without interrupting for ~60–90 seconds, summarize in your words, and use teach-back to verify understanding. Teach-back (“Just to be sure I explained it clearly, could you tell me how you’ll take the medicine?”) turns a monologue into a partnership and catches misunderstandings before they become errors. It’s especially powerful for complex regimens, new diagnoses, and discharge instructions. As of August 2025, AHRQ’s Health Literacy Universal Precautions Toolkit (3rd ed.) offers practical scripts, signage, and forms to normalize teach-back across teams. Meta-analyses and reviews suggest teach-back improves comprehension and self-management, and some studies show reductions in utilization and readmissions when implemented systematically.
2.1 Steps you can steal today
- Ask: “What’s the top thing you need from today’s visit?”
- Reflect: “So the swelling started after your shift, and your main worry is missing work.”
- Teach-back: “How will you explain the red flag symptoms to your partner?”
- Document what the patient said (not just what you said), then message a 3-bullet recap.
2.2 Numbers & guardrails
- Aim for 1–2 teach-back checks per visit (discharge needs more).
- Keep explanations to <2 minutes per concept; chunk and check.
- Use 12–14 pt handouts with icons for key actions.
Synthesis: Listening creates the bond; teach-back proves it—turning empathy into safer, shared memory.
3. Share Decisions With Decision Aids
Empathy means sharing control when more than one reasonable option exists. Patient decision aids raise knowledge, align choices with values, and improve risk perception—across screening and treatment contexts. The 2024 Cochrane review (over 200 trials) found decision aids increase informed, values-congruent choices and active participation, with no harms noted. Use them to structure conversations about PSA screening, statins for primary prevention, birth options, or knee osteoarthritis. Combine a concise “options, benefits, harms” summary with a one-page values clarification exercise; then ask, “What outcomes matter most if we fast-forward two months?” Decision aids don’t replace you; they frame a more human discussion.
3.1 How to do it
- Introduce the choice explicitly and check readiness to decide.
- Offer a trusted decision aid (e.g., Ottawa Hospital Research Institute inventory) and review together.
- Ask a values question (“What trade-off are you most unwilling to make?”), then decide or plan a follow-up. decisionaid.ohri.ca
3.2 Mini checklist
- Use neutral language; avoid steering.
- Quantify absolute risks with icon arrays.
- Document the decision and the values that drove it.
Synthesis: Decision aids operationalize respect—patients feel heard because the process honors what matters to them. Cochrane
4. Practice Trauma-Informed Care
Trauma—past or recent—shapes how patients perceive, remember, and act in healthcare. Trauma-informed care (TIC) asks, “What happened to you?” not “What’s wrong with you?” The SAMHSA framework outlines six principles: safety; trustworthiness & transparency; peer support; collaboration & mutuality; empowerment, voice & choice; and cultural, historical & gender issues. In practice: explain why you’re doing each step, offer choices (door open/closed, gowned/blanketed), and avoid surprise touch. TIC is empathy at the systems level—policies and spaces that reduce re-traumatization while preserving clinical excellence. Small shifts—like narrating your exam or asking consent for each maneuver—change the body language in the room.
4.1 How to implement
- Before: Screen for triggers only when resources exist; set expectations: “I’ll explain each step and you can pause me anytime.”
- During: Offer two choices when possible; validate emotion before education.
- After: Share a simple safety plan and supports.
4.2 Region notes
- Align with local safeguarding laws and reporting duties.
- Document consent/refusal clearly; provide chaperones per policy.
Synthesis: TIC converts empathy from a momentary gesture to a durable sense of safety that patients can count on.
5. Make Care Culturally Responsive—and Use Professional Interpreters
Empathic care honors language and culture. The U.S. National CLAS Standards and Joint Commission guidance emphasize effective communication and cultural competence; professional interpreters reduce errors and improve outcomes for patients with limited English proficiency. Avoid family-as-interpreter except for emergencies; brief the interpreter, speak to the patient directly, and pause for complete interpretation. Use respectful, person-first language and ask about health beliefs (“What do you call this problem?”). Build a small phrase bank for rapport in common languages, but switch to a certified interpreter for clinical content.
5.1 Quick practice tips
- Pre-brief: goals, sensitive terms, tempo.
- Talk in short, complete thoughts; avoid jargon.
- Check understanding with teach-back through the interpreter.
5.2 Evidence snapshot
Systematic reviews report better communication quality and, in many studies, better clinical outcomes when professional interpreters are used compared with ad-hoc approaches. PubMed
Synthesis: Language access isn’t a courtesy; it’s core empathy—and a patient safety requirement in many settings.
6. Design for Health Literacy and Numeracy
Even highly educated patients can struggle with medical prose, numbers, and next steps—especially when stressed. Treat low health literacy as the default: use plain language, short sentences, and meaningful headings; replace decimals and relative risks with whole numbers and visuals. AHRQ’s Health Literacy Universal Precautions Toolkit (3rd ed.) provides ready-to-use materials for spoken and written communication, self-management, and supportive systems. In clinic, present one message at a time, prioritize no more than three actions, and document the plan in a 3-bullet message with icons. These seemingly small tweaks convert empathy into behaviors that patients recognize as respect.
6.1 Mini checklist
- Use “need to know / need to do” format.
- Prefer absolute risks (5 in 100) over percentages when possible.
- Replace dense blocks with icons and white space; print at 12–14 pt minimum.
6.2 Tools & examples
- Plain-language medication plans.
- Icon arrays for screening decisions.
- Color-coded inhaler action plans.
Synthesis: Health-literate design is empathy you can see on paper—and patients can act on at home.
7. Let Your Body Say “I’m With You”: Nonverbal Presence & Environment
Empathy is physical: sit at eye level, soften your shoulders, let silence do some work, and (with consent) use supportive touch. Studies show sitting changes how time is perceived; patients often feel you spent longer with them and listened more carefully when you’re seated. Add environment: reduce noise, dim harsh lights, close the door for privacy, and ensure a clear line of sight. In training, practice micro-skills on video: camera at eye height, warm lighting, distractions removed. These tweaks reframe the interaction from transactional to relational—even when the visit is short.
7.1 Practical moves
- Seat first, then greet by name, then ask your opening question.
- Keep your hands still when listening; nod and paraphrase.
- Use one beat of silence after delivering key information.
7.2 Mini case
An ED physician starts the consult seated. The patient later reports the doctor “stayed longer,” though the timestamp shows five minutes. The perception shift came from posture and pacing, not duration.
Synthesis: Your posture, pace, and place are the first language patients read; make them say “you matter.”
8. Validate Pain and Symptoms—and Align on Function Goals
Patients with pain and other subjective symptoms need fast validation: “I believe you, and I want to help.” Empathy here is not just kindness; it correlates with better outcomes in chronic low back pain and other conditions. Recent cohort data (2024) found higher physician empathy (CARE Measure) associated with lower pain intensity, less disability, and better quality of life over 12 months—outperforming some common therapies. Use a functional goal (walk to the mailbox, sleep through the night) to anchor decisions. Invite patients to rank outcomes (pain relief, function, side effects), and review progress at set intervals.
8.1 How to do it
- Start with validation and a functional goal.
- Discuss a multimodal plan: movement, sleep hygiene, topical/systemic options, pacing.
- Reassess in 2–4 weeks; adjust based on the patient’s lived data.
8.2 Numbers & guardrails
- Use 0–10 pain plus function scales (e.g., RMDQ) at baseline and follow-up.
- Avoid implying disbelief when imaging is normal; explain pain physiology.
Synthesis: Validating pain turns confrontation into collaboration; function-first plans help patients feel seen and supported. PMC
9. Use Motivational Interviewing to Unlock Behavior Change
When the task is behavior change—tobacco, diet, exercise, adherence—Motivational Interviewing (MI) blends empathic listening with strategic questions that surface a patient’s own reasons to change. Evidence is mixed across conditions, but reviews show MI can improve medication adherence and support smoking cessation, with modest effects on some cardiometabolic risks. Keep it brief and focused: ask open questions, reflect change talk, and end with a small, specific step the patient chooses. MI respects autonomy while amplifying hope. Wiley Online Library
9.1 MI micro-skills (OARS)
- Open questions: “What would a good week of meds look like for you?”
- Affirm: “You kept walking even when it hurt—that’s grit.”
- Reflect: “On one hand you want to quit, and on the other cigarettes help with stress.”
- Summarize: tie their reasons to a next step.
9.2 Mini example
Patient unsure about statins sets a goal to try a 2-week adherence experiment with a pillbox and text reminder, then decides based on muscle-symptom diary and lipid changes. Oxford Academic
Synthesis: MI is empathy with a vector—it moves with the patient’s motivation, not against it. SciELO Public Health
10. Show Digital Empathy in Telehealth & Portals
Empathy translates on screens when you manage “webside manner.” Stabilize tech (camera at eye level, good audio), look at the lens when listening, and narrate your clicks so patients don’t feel ignored. Research and expert guidance emphasize intentional rapport on video—warm greeting, brief agenda, explicit pauses for questions—and show that patients’ relationship-centered experience can be preserved with good digital etiquette. In portal messaging, use short paragraphs, normalize emotions, and include one clear action. End video visits with a verbal summary and a portal recap within the hour. JMIR
10.1 Quick checklist
- Eye-level camera, minimal background, confirm privacy.
- Start with “What would make this visit successful for you?”
- Share screen to review imaging or decisions; send a summary message.
10.2 Access & equity
Not every patient has bandwidth, devices, or privacy; offer phone or in-person alternatives and assist with setup. jopm.jmir.org
Synthesis: Telehealth empathy is deliberate—it’s how you use the channel, not the channel itself, that keeps patients feeling connected. American Medical Association
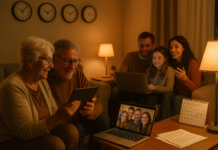
11. Partner With Family Caregivers—Within Consent & Law
Empathy extends to the patient’s care network. Many patients want a family member or friend involved—at bedside, on rounds, or during video visits. Done well, caregiver partnership boosts safety and continuity; AHRQ resources on patient-family engagement and family-centered rounds show how to invite families into care planning. Balance this with confidentiality: in the U.S., HIPAA allows sharing relevant information with individuals involved in care when the patient agrees or does not object; in the U.K., NHS guidance likewise supports appropriate sharing with carers with consent, and information governance frameworks clarify exceptions when patients cannot consent. Build a routine: ask who the patient wants present, capture names in the chart, and document preferences for information sharing.
11.1 How to do it
- Ask every patient: “Who do you want involved in your care decisions?”
- If yes, document names and contact details; confirm what can be shared.
- Offer family-centered rounds or invite caregivers to the last five minutes of visits.
11.2 Guardrails & region notes
- U.S.: Follow HIPAA 45 CFR 164.510(b) and your facility policy; use proxies when appropriate.
- U.K.: Share with carers when there is consent or in best interests if the patient lacks capacity; document rationale. HHS.govNHS England Digital
Synthesis: Families are often the continuity of care; set clear consent boundaries and harness their strengths to sustain empathy at home.
FAQs
1) What exactly is “empathy in healthcare,” and how is it different from sympathy?
Empathy is understanding a patient’s emotions and perspective and responding in ways that convey that understanding; sympathy is feeling for someone, which can unintentionally center the caregiver’s feelings. In practice, empathy sounds like naming emotion and aligning on next steps, while sympathy risks reassurance without action. Tools like NURSE help keep the focus on the patient’s experience.
2) Does empathy really change outcomes, or just satisfaction scores?
Beyond experience scores (e.g., HCAHPS), studies associate physician empathy with improved clinical outcomes in chronic pain—lower pain intensity, less disability, and better quality of life over 12 months. While causality is complex, the signal is consistent enough to justify training and measurement.
3) How can I show empathy when I’m short on time?
Use micro-skills: sit, ask one open question, reflect in one sentence, name the emotion, and agree on one next step. Evidence suggests even posture (sitting) shifts patient perceptions of time and listening. Script your first 60–90 seconds, then let the patient speak uninterrupted. PubMed
4) What tools can I use to measure empathy?
The Consultation and Relational Empathy (CARE) Measure is a validated 10-item patient-rated tool used in primary care and beyond. It’s short, free for many uses, and has been adapted internationally. PubMedcaremeasure.stir.ac.uk
5) Is teach-back condescending?
Not when framed as a test of the explanation, not the person. Try: “I want to be sure I explained this clearly—can you show me how you’ll use the inhaler?” AHRQ’s toolkit provides language for normalizing the practice across your clinic.
6) Are decision aids only for complex surgeries?
No. They’re useful anywhere there are meaningful options and trade-offs—screening tests, medications, birth options, palliative choices. The 2024 Cochrane review shows decision aids increase knowledge and values-aligned choices across a wide range of decisions. PubMed
7) When should I use a professional interpreter?
Any time language barriers could affect understanding. Systematic reviews show professional interpreters reduce errors and improve outcomes compared with ad-hoc solutions. Brief them before the visit and speak directly to the patient.
8) How do I adapt telehealth for empathy?
Manage “webside manner”: eye-level camera, good lighting, explicit agenda, narrate your clicks, and summarize at the end. Evidence and expert guidance indicate relationship-centered care can be preserved with deliberate techniques.
9) What about patients with trauma histories?
Use trauma-informed care: emphasize choice and safety; explain before you touch; validate emotion; and let patients pause the exam. SAMHSA’s framework outlines six principles that map directly to empathic practice. ScienceDirect
10) Can empathy reduce malpractice risk?
While this article doesn’t make legal claims, better communication and shared understanding generally reduce misunderstandings and conflict. Focus on transparency, teach-back, and clear documentation—best practices recommended by safety agencies. PSNet
11) How do I involve family without breaching privacy?
Ask who the patient wants involved, document it, and share information relevant to that involvement. Follow HIPAA (U.S.) or NHS guidance (U.K.) and your local policy; when patients lack capacity, share in their best interests and document your reasoning.
12) What team tools support empathic, safe care?
Use TeamSTEPPS communication tools (e.g., SBAR) and standardized handoffs like I-PASS; both improve communication quality, and I-PASS is associated with reduced medical errors in multicenter studies. Empathy travels better when the team is aligned.
Conclusion
Empathy isn’t a soft extra—it’s a clinical skill and team habit that makes care safer, decisions wiser, and relationships sturdier. Across settings—bedside, clinic, telehealth—patients chiefly remember how we listened, what we validated, and whether we partnered with their goals and families. The strategies in this guide convert empathy from intention to practice: frameworks (NURSE, SPIKES) to respond to emotion; teach-back and decision aids to create shared understanding; trauma-informed and culturally responsive routines that make safety felt; and measurable behaviors (sitting, pausing, summarizing) that patients experience as presence. Build small rituals into your day: start seated, ask one open question, reflect once, name the emotion, agree on one next step, and send a short recap. Then scale with team tools (SBAR, I-PASS), interpreters, and family-centered processes. Empathy is the thread that holds these together—and the bond patients carry home.
Ready to start? Choose one strategy above and make it standard in your next five encounters.
References
- SPIKES—A Six-Step Protocol for Delivering Bad News, The Oncologist (Baile WF et al.), 2000. Renaissance School of Medicine
- Responding to Emotion: NURSE Statements, VitalTalk, page updated 2025. vitaltalk.org
- Health Literacy Universal Precautions Toolkit (3rd ed.), Agency for Healthcare Research and Quality, 2023. AHRQ
- Decision Aids for People Facing Health Treatment or Screening Decisions, Cochrane Review (Stacey D. et al.), 2024. Cochrane Library
- National Standards for Culturally and Linguistically Appropriate Services (CLAS), HHS Office of Minority Health, 2023. https://thinkculturalhealth.hhs.gov/clas/standards PMC
- Do Professional Interpreters Improve Clinical Care for Patients with Limited English Proficiency? Health Services Research (Karliner LS et al.), 2007; and AHRQ PSNet summary, 2011. ; PMCPSNet
- Physician Empathy and Chronic Pain Outcomes, JAMA Network Open, 2024. JAMA Network
- HCAHPS: Patients’ Perspectives of Care Survey, Centers for Medicare & Medicaid Services, updated June 3, 2025. Centers for Medicare & Medicaid Services
- To Succeed With Telehealth, Know Your “Webside Manner”, American Medical Association, 2020; and Enhancing Your Webside Manner, Cleveland Clinic Journal of Medicine (Modic MB), 2021. ; American Medical AssociationPMC
- Family-Centered Rounds Toolkit & Guide to Patient and Family Engagement, AHRQ, 2017–2025. ; https://www.ahrq.gov/patient-safety/patients-families/patient-family-engagement/index.html AHRQ
- HIPAA—Disclosures to Family and Friends Involved in Care, HHS OCR, 2022; NHS England Sharing Information With Unpaid Carers, 2022. ; HHS.govNHS Transformation Directorate
- Sitting at the Bedside—Patients’ Perception of Time Spent, Patient Education and Counseling (Swayden KJ et al.), 2012; When Doctors Sit, Patients Understand, BMJ, 2023. https://pubmed.ncbi.nlm.nih.gov/21640550/ ; https://www.bmj.com/content/383/bmj-2022-074193 PubMed
- TeamSTEPPS: SBAR & Communication Tools, AHRQ, 2023; I-PASS Handoff Program—NEJM multicenter study, 2014. ; AHRQNew England Journal of Medicine