Blazing summer days don’t just feel uncomfortable—they raise the stakes for dehydration, heat exhaustion, and heat stroke. This guide gives you clear, practical hydration steps for hot climates, whether you’re commuting, training, working outdoors, or exploring on holiday. You’ll learn how much to drink, when to add electrolytes, how to pair fluids with cooling, and how to adapt for kids, older adults, and fasting days. In short: in hot weather, hydration means matching your sweat losses with fluid and electrolytes while pacing activity and using shade and cooling. Aim to prevent >2% body mass loss, keep urine pale, and avoid drinking faster than your body can absorb (generally not more than about 1 quart/1 liter per hour).
Quick start (skim list): Measure your sweat rate; prehydrate; sip steadily; include sodium when sweating heavily; use cold fluids and shade; track urine color and body mass; don’t exceed ~1 L/hour; plan routes and refill points; acclimatize over 1–2 weeks; tailor strategies for vulnerable groups.
Medical note: This article is educational, not medical care. If you have kidney, heart, or endocrine conditions, are pregnant, or take diuretics, ask your clinician how to personalize these steps.
1. Know Your Sweat Rate—and Turn It Into a Drinking Plan
Start by estimating how much you actually sweat; then let that number shape your intake. Most adults in heat lose roughly 0.5–2.0 liters per hour, but personal rates vary with body size, pace, humidity, and acclimatization. The best way to cut through guesswork is to weigh yourself before and after a representative 60–90 minute session in similar heat. Each kilogram (2.2 lb) of body mass lost equals about 1 liter of fluid lost, minus any fluid you drank and plus urine you produced. Aiming to limit body mass loss to <2% helps maintain performance and reduce heat strain; more than that raises risk for heat illness. Use this test to set a target drinking rate you can actually tolerate, keeping in mind that GI comfort caps most people near 0.4–1.0 L/hour.
1.1 How to do it
- Weigh before (minimal clothing), track fluids consumed, track urine, weigh after.
- Sweat rate (L/h) ≈ [(Pre − Post) kg + drinks (L) − urine (L)] ÷ hours.
- Target intake during similar heat ≈ 60–80% of that rate to start; adjust by feel and urine color.
1.2 Numbers & guardrails
- Keep body mass loss <2% on hot days.
- Most people absorb ≤1.0 L/hour without discomfort.
- Re-check sweat rate when weather or pace changes.
Synthesis: A 20-minute bathroom scale session pays off all summer: you’ll drink with purpose instead of guessing.
2. Use Electrolytes Strategically—Especially Sodium
Electrolytes replace what sweat removes, help you retain the fluid you drink, and reduce cramping risk during heavy sweat days. Sodium is the workhorse here; potassium matters too, but hot-weather cramps often track with sodium deficits. For routine errands and light activity, water and normal salty meals are usually enough. For long, sweaty sessions (≥60–90 minutes, or if you’re a salty sweater with visible salt marks), add sodium via a sports drink (typically 300–700 mg/L) or a measured oral rehydration solution (ORS). ORS is not just for illness—it’s a precise, science-backed way to move water from gut to blood quickly when you’re behind.
2.1 Tools/Examples
- Sports drink: 4–8% carbs with sodium for long, sweaty sessions.
- ORS (WHO formulation): 75 mmol/L sodium + 75 mmol/L glucose; fast absorption when you’re depleted.
- Salty foods: Soup, broth, salted nuts, pickles with water if you prefer food-first.
2.2 Common mistakes
- Relying only on plain water during multi-hour sweat; over time this dilutes sodium.
- Guessing with “pinches of salt.” Use labeled products or recipes.
- Over-sugary drinks that slow absorption and upset the stomach.
Synthesis: Match your drink to your sweat: heavier sweat and longer duration call for sodium, not just more water.
3. Prehydrate Smartly Before Heat Exposure
Prehydration tops up plasma volume and lowers heart strain in the heat. A practical plan: in the 2–3 hours before outdoor work, errands, or training, drink ~5–7 mL/kg (about 350–500 mL for a 70 kg adult), then sip another 200–300 mL 20–30 minutes before you start. If you’re a salty sweater or the day is very hot/humid, include some sodium (e.g., a lightly salted snack or electrolyte tablet) to help retain that fluid. The goals: start euhydrated, have normal urine output, and avoid a sloshy stomach.
3.1 Mini-checklist
- 2–3 hours before: 350–500 mL fluids; include a little sodium.
- 20–30 minutes before: 200–300 mL cool water or electrolyte drink.
- Check urine: pale = likely good to go.
3.2 Region note (humid vs. dry heat)
In humid monsoon conditions (e.g., Karachi in July–August), sweat evaporation is impaired, so prehydration and shaded rest periods matter even more than in dry deserts where sweat evaporates efficiently.
Synthesis: Arrive at the heat already “topped up,” not playing catch-up in the first hour.
4. Sip Steadily and Pair Fluids With Rest–Shade Cycles
Hydration works best when paired with heat management: shade, airflow, and planned breaks. Instead of chugging intermittently, take small, regular sips and use scheduled pauses (e.g., every 20–30 minutes) to cool down. Occupational guidance stresses water–rest–shade and recognizes that risk depends on both heat exposure and workload; for those who can, use Wet Bulb Globe Temperature (WBGT) or at least Heat Index to plan work/rest ratios. If you don’t have a WBGT meter, the OSHA–NIOSH Heat Safety Tool app gives risk guidance by Heat Index and protective actions. Wikipedia
4.1 Practical steps
- Pre-schedule short, shaded breaks; set phone reminders.
- Use fans or natural breezes to boost evaporation.
- Keep a full bottle in reach; a visible cue increases sips.
4.2 Numbers & guardrails
- Hot days raise risk faster in direct sun; Heat Index can read ~8 °C (15 °F) higher in full sun than in shade.
- Don’t try to “outrun” heat with only water—pair it with cooling and time-outs. National Weather Service
Synthesis: Hydration is necessary but not sufficient; combine steady sipping with planned cooling to actually lower strain.
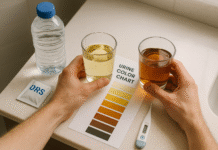
5. Track Urine, Body Mass, and Symptoms (and Avoid Overdrinking)
Your body gives useful signals: pale straw-colored urine generally suggests adequate hydration, while dark, strong-smelling urine, dizziness, headache, and fatigue warn you’re behind. On long, hot days, weigh before/after demanding outings to catch >2% losses. Just as important: don’t overdrink. Rapidly consuming more than ~1 quart (~1 L) per hour can cause dangerous hyponatremia, especially if you’re not eating salty foods alongside. The sweet spot is to replace most—not necessarily all—sweat losses during activity, then finish the job with food and fluids after.
5.1 Mini-checklist
- Urine pale = probably okay; dark = drink more.
- Aim body mass change: within 0–2% by day’s end.
- Cap intake near 1 L/hour unless a clinician tells you otherwise.
5.2 Common pitfalls
- “Clear pee all day” chasing: can mean overdoing water.
- Skipping sodium during all-day sweating.
- Ignoring early symptoms because you’re “almost done.”
Synthesis: Use simple indicators to steer between dehydration and overhydration.
6. Make Cold Fluids and Cooling Your Allies
Cold drinks empty from the stomach about as well as cool ones and can reduce perceived effort; ice slurries can pre-cool the body and improve endurance in the heat, particularly when full-body immersion isn’t practical. Combine cold fluids with other practical coolers: a wet scarf or cooling towel on the neck, misting fan, shaded stops, and evaporative cooling from loose, breathable clothing. In field settings without access to baths or AC, the pairing of ice slurries or very cold fluids plus shade and airflow is a realistic, high-return option.
6.1 How to do it
- Freeze a half-filled bottle; top up before heading out.
- Pack an insulated bottle; refill with ice where possible.
- For long sessions: alternate steady sips with brief shade breaks.
6.2 Mini case
- 75 kg runner in 35 °C: ice slurry (7–10 g/kg over ~20–30 minutes) before a 60-minute run + sips during may feel noticeably easier versus lukewarm water alone.
Synthesis: Cold fluids and simple cooling tactics work together to buy you comfort and safety when the mercury spikes.
7. Eat Your Water—and Your Salt
Food can provide ~20% of total water intake on a typical day, and it’s an easy way to add sodium without over-salting drinks. In hot spells, emphasize high-water foods (watermelon, cucumbers, oranges, tomatoes, yogurt, soups) and include modestly salty items (broths, olives, salted nuts) when you’re sweating more than usual. This food-first pattern supports hydration, improves palatability, and reduces the risk of drinking excessive plain water with too little sodium. Tea and coffee can count toward your daily fluid, too—just avoid loading them with sugar and be mindful of caffeine sensitivity. National Academies Press
7.1 Quick picks
- Water-rich: Watermelon, cucumber, citrus, tomatoes, lettuce, yogurt.
- Salty add-ons: Broth-based soups, pickles, salted nuts, cheese.
- Smart drinks: Plain or sparkling water, diluted juice, unsweetened tea.
7.2 Common mistakes
- Relying only on sweet drinks (gut upset, tooth decay).
- “Low-sodium everything” on heavy-sweat days.
- Skipping meals—missed electrolytes and fluids.
Synthesis: Let meals carry part of the load: water + electrolytes + nutrients = sustainable hydration.
8. Plan Around the Heat: Timing, Routes, and Refills
The simplest hydration boost is avoiding the worst heat. In many hot regions, early morning and late evening are dramatically safer. If you must be out midday, shorten outings and build in shade and indoor pit stops. Pre-map water sources: parks, masjids/temples with taps, cafes, and public fountains. For city commutes, carry a 750–1000 mL insulated bottle and set calendar nudges to refill. For day hikes or fieldwork, pre-cache water, set crew check-ins, and bring a lightweight filter if you’ll rely on non-potable sources.
8.1 Mini-checklist
- When: Start early/late; avoid 11:00–16:00 where possible.
- Where: Choose shady sides of streets; add indoor cool-downs.
- What: Carry enough for the longest stretch without refills + one extra.
8.2 Tools
- Heat Index/WBGT apps for planning rest and pace; pick shaded, breezy routes. As of August 2025, the OSHA–NIOSH Heat Safety Tool and NWS calculators are the most widely referenced public tools. wpc.ncep.noaa.gov
Synthesis: Strategy beats willpower—plan the when/where so your bottle and the weather are on your side.
9. Choose the Right Drink: Water vs. Sports Drink vs. ORS (and What About Caffeine?)
Think of drinks as tools. Water is perfect for short, light activity and most daily life. Sports drinks shine in longer, sweatier efforts: they add carbs (4–8%) and sodium to improve palatability and retention. ORS is a clinical-grade formula for rapid rehydration when you’re notably behind (e.g., after heat illness, GI upset, or heavy-sweat deficits); it’s saltier than sports drinks and not designed as your all-day sip. Caffeine? Moderate tea/coffee can count toward fluid; just avoid large, sweet, highly caffeinated drinks before long heat exposure if they upset your stomach or your sleep. KHSAA
9.1 Quick guide
- Water: Routine; add a salty snack if sweat is heavy.
- Sports drink: Long/hot sessions; when sweat is visibly salty.
- ORS: Catch-up after big deficits; not a flavor-first option.
9.2 Common myths
- “Coffee dehydrates you.” Habitual moderate intake doesn’t negate hydration; it still contributes to daily fluids.
- “Coconut water is the perfect sports drink.” It’s low in sodium; fine as a beverage, not ideal for salt-heavy sweat.
Synthesis: Match the drink to the job. Water for routine, sports drink for long heat, ORS for recovery.
10. Carry the Right Gear (and Use It)
A little kit solves a lot of problems: an insulated bottle to keep fluids cool; a soft-flask or hydration pack for hands-free sipping; a few electrolyte packets; a lightweight cap with a brim; and a small microfiber towel you can soak for evaporative cooling. If you’ll be away from safe taps, carry a filter or purification tablets. On commutes, stash a spare bottle at work or in your bag; in the field, stage a cooler in the shade. Small friction-reducing habits—like pre-chilling bottles and labeling them with tick marks every 250 mL—keep you on pace without thinking.
10.1 Mini-checklist
- 750–1000 mL insulated bottle; pre-chill.
- Electrolyte packets (clearly labeled sodium content).
- Cooling towel/neck wrap; brimmed hat; light, breathable clothing.
10.2 Region note (travel & water safety)
Traveling where tap water isn’t safe? Use sealed bottles, avoid unsafe ice, and consider a portable filter. When in doubt, treat or boil water and prioritize ORS if you get behind.
Synthesis: Gear makes hydration automatic; prepare once so you don’t improvise when it’s hottest.
11. Acclimatize Over 1–2 Weeks and Recheck Your Plan
Heat acclimatization improves sweat rate, reduces sodium losses, lowers heart rate, and makes the same work feel easier. Build it gradually over 7–14 days—especially if you’re new to heat or returning after time away. A simple rule used in occupational settings: on day one, do ~20% of your usual hot-weather duration, then add ~20% per day until you reach your normal load. Even after you acclimatize, a week away from heat can “fade” adaptations; re-ramp for a few days. Reassess sweat rate when conditions change.
11.1 How to do it
- Days 1–5: Shorter sessions in the heat with generous shade and fluids.
- Days 6–10: Extend time; introduce modest workloads.
- Maintain: Keep some heat exposure each week in summer.
11.2 Common mistakes
- “Jumping back in” after travel or illness.
- Assuming AC breaks erase gains (they don’t).
- Not adjusting sodium as sweat rate rises with acclimatization.
Synthesis: Give your body time to adapt; your hydration plan will work better once you do.
12. Tailor Hydration for Kids, Older Adults, Pregnancy, Fasting, and Chronic Conditions
Some groups need modified plans. Children heat up faster and may not recognize thirst—offer frequent fluids and cooling breaks. Older adults may have reduced thirst sensitivity and take medications that complicate fluid balance—schedule drinks and monitor closely in heat waves. Pregnancy increases fluid needs; keep caffeine ≤200 mg/day and prioritize cool environments. Fasting (e.g., Ramadan) in summer calls for “bookend hydration”: pre-dawn ORS/salted foods and post-sunset rehydration, careful daytime pacing, and shade. Chronic kidney/heart disease or diuretic use changes everything—ask your clinician for personalized limits and signs to stop.
12.1 Mini-checklist by group
- Kids: Offer fluids every 20–30 minutes in heat; choose water/milk; avoid high-sugar drinks.
- Older adults: Set alarms; pair sips with routine tasks; cool rooms to reduce sweat.
- Pregnancy: Frequent small sips; limit caffeine; add ORS if behind.
- Fasting: Front-load at suhoor/iftar; keep activity cooler/darker; monitor symptoms.
Synthesis: The core rules stay the same—match fluid + sodium to sweat and pace the day—but the margins of safety are narrower, so plan proactively. CDC
FAQs
1) How much should I drink on a very hot day?
There’s no single number that fits everyone. Start with your sweat rate test and plan to replace most (not all) losses during activity, then finish rehydrating with meals and fluids afterward. Many people tolerate 0.4–1.0 L/hour during sustained heat; don’t exceed ~1 L/hour unless advised by your clinician. Keep body mass loss under 2% and urine pale.
2) Do tea and coffee count toward hydration?
Yes—unsweetened tea and coffee can contribute to total fluid, especially if you’re a regular consumer. They’re not “dehydrating” in moderate amounts, but avoid large sugary or highly caffeinated drinks if they upset your stomach or sleep before heat exposure.
3) When do I need electrolytes instead of water?
If you’re sweating for 60–90 minutes or more, you see salt marks on clothing, get muscle cramps, or feel “sloshy” from lots of plain water, add sodium via a sports drink or ORS. Use ORS when you’re meaningfully behind (after heavy sweat, illness, or heat illness).
4) What’s the difference between Heat Index and WBGT?
Heat Index combines temperature and humidity to estimate “feels-like” temperature in shade/light wind; WBGT adds sun (radiant heat) and wind to gauge heat stress for active people. If you can, use WBGT; otherwise, Heat Index tools and apps still help plan rest–shade.
5) Are ice-cold drinks or ice slurries safe?
Yes for most people; they can reduce perceived exertion and help pre-cool. If cold causes stomach upset, use cool fluids and external cooling (wet towel, misting fan, shade).
6) How do I spot early dehydration vs. overhydration?
Dehydration: thirst, dark urine, headache, dizziness, fatigue. Overhydration/hyponatremia: nausea, bloating, headache, confusion; often after drinking large volumes of low-sodium fluid. Cap intake near 1 L/hour and include sodium on heavy sweat days. Seek urgent care for severe symptoms.
7) Is coconut water a good sports drink?
It’s hydrating and contains potassium, but it’s relatively low in sodium. For long, sweaty efforts you’ll replace sodium better with a sports drink or salty snacks plus water. Use coconut water for variety, not as your primary “salt” source.
8) What about “drink to thirst” vs. scheduled drinking?
Both can work. In casual heat exposure, drinking when thirsty is fine. In long, hot, or high-stakes settings (worksites, long runs), thirst can lag behind needs—use your sweat rate and a schedule, then adjust based on urine color and how you feel.
9) How long does heat acclimatization take?
Typically 7–14 days. Start with shorter heat exposures and add ~20% time each day. If you’ve been away from heat for a week or more, rebuild over a few days. CDCOSHA
10) I’m traveling where tap water isn’t safe. How do I hydrate?
Use sealed bottled water, avoid unsafe ice, and consider a portable filter or boiling water. Keep ORS on hand; if you get GI illness, rehydrate aggressively and seek care if severe.
Conclusion
Summer heat raises the bar for hydration, but you don’t need guesswork or gimmicks. Measure your sweat rate once and build a plan you can execute: prehydrate before the heat, sip steadily, and include sodium when the sweat is heavy. Pair fluids with rest–shade cycles, use cold drinks and simple cooling tricks, and plan your routes for refills and breezes. Over one to two weeks, acclimatize so the same workload feels easier and safer, and adjust for the people who need the most care—kids, older adults, pregnant people, and those fasting or managing chronic conditions. If you remember just three things, make them these: replace most—but not all—sweat during activity, keep urine pale, and never push beyond ~1 liter per hour without medical guidance. Your next step: pick tomorrow’s hottest task, set a refill route, and pack one electrolyte option—then feel the difference by day’s end.
Copy-ready CTA: Beat the heat smarter—measure your sweat rate this week and build your personal hydration plan.
References
- American College of Sports Medicine Position Stand: Exercise and Fluid Replacement, ACSM / Medicine & Science in Sports & Exercise, 2007. https://pubmed.ncbi.nlm.nih.gov/17277604 PubMed
- Water, drinks and hydration, NHS, page last reviewed May 17, 2023. nhs.uk
- OTIEC Course 501 – Water Intake Guidance (“Do not drink more than 1 quart per hour”), OSHA Training Materials, accessed 2025. https://www.osha.gov/otiec/course/501-train/materials/water-intake koreystringer.institute.uconn.edu
- OSHA–NIOSH Heat Safety Tool App, NIOSH/CDC, updated Aug 27, 2024. CDC
- Heat Index – JetStream, NOAA/National Weather Service, Sept 20, 2023. NOAA
- Pre-cooling for endurance exercise performance in the heat: a systematic review, BMC Medicine, 2012. BioMed Central
- Dietary Reference Intakes for Water, Potassium, Sodium, Chloride, and Sulfate – Chapter 4 (Water), National Academies (IOM), 2005. National Academies Press
- Calculate Sweat Rate (formula/worksheet), CDC (archived resource), accessed 2025. CDC
- OSHA Heat – Heat Safety Tool (overview), OSHA, accessed 2025. OSHA
- WHO/UNICEF: Reduced-Osmolarity Oral Rehydration Salts (ORS) – Composition and Rationale, WHO IRIS technical updates (e.g., WHO_FCH_CAH_06.1), 2006. WHO Apps
- Key Facts About Extreme Heat (vulnerable groups and protection), CDC, updated 2024. https://www.cdc.gov/nceh/features/extremeheat/index.html CDC
- Traveler’s Health: Food & Water Safety, CDC Yellow Book portal, updated 2024. https://www.cdc.gov/travel/page/food-water-safety CDC