If your energy, mood, or performance fall off a cliff, dehydration is a common—often overlooked—reason. Dehydration happens when fluid losses exceed intake, leaving your body short on water and electrolytes it needs for temperature control, blood pressure, digestion, and brain function. The fastest way to confirm you’re running low is to check urine color, thirst, and how you feel after drinking. Quick answer: drink water or an oral rehydration solution (ORS), cool down, and rest; seek urgent care for confusion, fainting, or signs of heat stroke. As a general frame, many adults meet needs around 3.7 L/day (men) and 2.7 L/day (women) from all beverages and foods, though individual needs vary with heat, activity, and health.
Quick rehydration steps (at a glance)
- Sip 300–500 mL water now; if you’ve had heavy sweating, choose ORS.
- Move to shade/AC; loosen clothing; place cool cloths on neck, armpits, groin.
- Eat something salty (e.g., broth, salted crackers) if you’ve been sweating a lot.
- Check urine in 30–60 minutes; aim for pale straw color.
- If symptoms worsen (confusion, fainting, hot/dry skin, fever), seek emergency care.
Medical disclaimer: This guide is educational and not a diagnosis. For infants, older adults, pregnancy, chronic illness, or persistent/Severe symptoms, contact a clinician or emergency services.
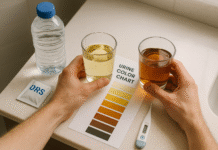
1. Dark Yellow Urine or Peeing Less Than 3–4 Times a Day
Dark, strong-smelling urine and infrequent urination are among the earliest, most reliable everyday signs of dehydration. If you’re peeing only a few times in a long workday, or your urine looks apple-juice colored instead of pale straw, your kidneys are concentrating fluid to conserve water. This usually pairs with thirst, a dry mouth, and sometimes a mild headache. While some supplements (like B-vitamins) can temporarily tint urine, a consistent dark color—especially with dryness, fatigue, or dizziness—should prompt you to drink more. Aim to see lighter color within an hour of rehydrating. For most people, a pale straw color suggests adequate hydration; extremely clear urine for long periods may mean overhydration.
1.1 Why it matters
- Urine color correlates with hydration markers like urine osmolality and specific gravity in healthy adults.
- Less frequent urination (e.g., <3–4 times/day) often indicates low intake or higher losses (heat, exercise, diuretics).
- Persistently dark urine with other symptoms can precede more serious problems (low blood pressure, dizziness). PMC
1.2 How to fix it (mini-checklist)
- Drink 300–500 mL water now, then reassess color in 30–60 minutes.
- If you’ve sweated heavily, use an ORS (sodium + glucose) for faster absorption.
- Track frequency: most people urinate every 3–4 hours when hydrated.
- Watch medications: diuretics and antihistamines can change output.
Bottom line: Use urine as your simple dashboard—pale straw color and steady frequency are your “hydrated” green lights.
2. Thirst, Dry Mouth, and Sticky Saliva
Thirst is your brain’s built-in alarm for rising blood osmolality; it often begins after modest water losses. If your mouth feels dry, your lips stick, or you crave fluids, that’s a practical call to drink. In office life, we often suppress thirst signals during meetings or commutes; by the time you finally drink, you may also notice fatigue or fogginess. In heat or with exercise, thirst may lag behind sweat losses, so relying only on thirst can under-shoot needs during prolonged effort. A simple rule: drink when thirsty in daily life, but plan ahead (carry a bottle, prehydrate) for heat and workouts.
2.1 Numbers & guardrails
- Mild dehydration around 1–2% body mass loss is enough to trigger thirst and degrade performance and mood.
- In hot/long exercise, schedule fluids rather than waiting for thirst alone.
2.2 How to fix it (step list)
- Take slow sips: 300–500 mL over 10–20 minutes.
- Moisten the mouth: sugar-free gum or a small rinse can reduce dry-mouth discomfort while you rehydrate.
- Prehydrate heat/workouts: ~500 mL about 2 hours before you start; then sip regularly.
Bottom line: Don’t overthink it—drink to thirst in everyday conditions and plan ahead for heat and long efforts.
3. Headache, Brain Fog, and Irritability
When you’re underhydrated, even slightly, you may develop a dull headache, slower reaction times, and trouble focusing. Studies in healthy women found that as little as ~1.3% dehydration worsened mood and concentration; broader reviews show cognitive performance slips at 1–2% dehydration. Many office headaches resolve with water, a light snack, cooling off, and a short break. If headaches persist, or you have neurologic red flags (confusion, weakness on one side, severe “thunderclap” pain), seek care immediately.
3.1 How to fix it (tools/examples)
- Immediate: 300–500 mL water + 1–2 salty crackers or broth if you’ve been sweating.
- Environment: lower room temperature, use a fan, take a brief walk.
- Track patterns: note if headaches follow long meetings, hot commutes, or intense workouts.
3.2 Mini case
During a summer deadline, you skip lunch and notice a band-like headache at 4 p.m. You drink 400 mL water, step into AC, and nibble a salty snack. Within 20–30 minutes the headache eases and focus returns—classic mild dehydration response.
Bottom line: If you’re foggy and tense by late afternoon, a water break and cooling usually help quickly.
4. Dizziness or Lightheadedness, Especially On Standing
Feeling woozy when you stand up is a hallmark dehydration signal. Low fluid volume can briefly drop blood pressure (orthostatic hypotension), making you dizzy, gray-out, or even faint. This risk rises in heat, after illness with vomiting/diarrhea, and in those on diuretics. Sit or lie down immediately if dizzy; elevating your legs can help blood return to the brain. If dizziness persists despite rehydration, or you faint, get medical care—it may reflect more than dehydration (e.g., arrhythmia, anemia).
4.1 How to fix it (checklist)
- Safety first: sit/lie down; don’t drive.
- Rehydrate: 300–500 mL water; if you’ve been sweating/ill, choose ORS.
- Cool down: shade/AC, cool cloths to neck/armpits/groin.
- Reassess in 15–30 minutes; seek care if symptoms persist or worsen.
4.2 Why ORS helps
Sodium-glucose co-transport in the small intestine speeds water absorption; low-osmolarity ORS (≈245 mOsm/L) is the global standard for rehydration.
Bottom line: Dizziness + heat or illness usually means “fluids now, feet up, and cool down.”
5. Unusual Fatigue and Exercise Feels Harder Than It Should
That run felt like quicksand? Dehydration reduces plasma volume, strains your heart, and makes exercise feel harder at the same pace. Even modest fluid deficits (≈2% body mass loss) impair aerobic performance and increase heat illness risk. Day to day, you’ll notice outsized fatigue during chores, a slow commute walk, or gym sets that normally feel fine. If effort skyrockets without another explanation (poor sleep, illness), check your hydration status and the day’s temperature/humidity.
5.1 How to fix it (plan)
- Before effort: ~500 mL 2 hours prior; small top-off 10–20 minutes pre-start.
- During effort: sip to limit body mass loss to <2%; use sports drink or ORS in prolonged heat.
- After effort: replace ~1.25–1.5 L per 1 kg body mass lost (includes food and drink); add sodium with meals.
5.2 Mini example
You weigh 70 kg pre-session and 68.6 kg after a hot run (-1.4 kg ≈-2%). Aim for ~1.75–2.1 L fluid over the next few hours with salty foods to fully rehydrate.
Bottom line: If everything feels harder, treat hydration as performance equipment—plan it.
6. Muscle Cramps and Weakness
Heat cramps and generalized muscle tightness commonly accompany dehydration and electrolyte shifts from sweat. Sodium losses are usually the main driver, but potassium can contribute. Cramps may hit during or after activity, especially in heat, and often respond to fluids + sodium and gentle stretching. Severe or persistent cramps, especially with dark urine and muscle pain, warrant medical evaluation to rule out rhabdomyolysis. CDC
6.1 How to fix it (steps)
- Stop, cool, and sip ORS or a sodium-containing sports drink.
- Stretch & massage the affected muscle; avoid aggressive loading.
- Replace salt in meals (soups, salted foods) for the next day if you’ve been sweating heavily.
6.2 Common mistakes
- Only drinking water after heavy sweat can dilute sodium too much; use electrolytes.
- Pushing through cramps increases injury risk.
Bottom line: Cramps in the heat are a loud hydration–electrolyte cue—treat both.
7. Dry, Cool, or Less Elastic Skin
Your skin can hint at your hydration status. While the old “skin pinch” (turgor) test isn’t perfect, dry or cool skin and delayed return after pinching over the forearm or abdomen can go along with dehydration—especially with other signs like thirst and dark urine. In heat, sweaty skin usually means you’re still producing sweat; as dehydration worsens (and with heat stroke), skin may become hot and dry. Do not rely on skin alone; always pair with urine and how you feel.
7.1 How to fix it (mini-checklist)
- Fluids first: water or ORS depending on sweat/illness.
- Environment: cool room, light/loose clothing.
- Moisturize: comfort measure only; it doesn’t rehydrate you internally.
7.2 Region note
In hot, humid climates, sweat evaporates less; you may look damp yet still be dehydrated. Use urine color/frequency and weight changes as objective checks.
Bottom line: Treat skin changes as supporting clues—confirm with urine and symptoms.
8. Fast Heartbeat, Shallow Breathing, or Palpitations
When your circulating volume drops, your heart compensates by beating faster to maintain blood pressure. You may notice palpitations, lightheadedness, or shortness of breath—especially when standing or climbing stairs. In moderate to severe dehydration, pulse rises and peripheral perfusion falls; if combined with confusion, chest pain, or fainting, seek urgent care. People with cardiovascular or kidney disease should be especially cautious during heat waves or illness.
8.1 How to fix it (now vs. later)
- Now: sit down, sip 300–500 mL water or ORS, and cool off.
- Later: review meds (diuretics), alcohol/caffeine, and your daily fluid plan; consider a clinician check if episodes repeat.
8.2 Numbers & monitoring
- Track resting pulse before/after rehydration; a noticeable drop after fluids/cooling supports volume depletion.
- For athletes, weigh pre/post sessions to keep loss <2% body mass.
Bottom line: A racing pulse is your body’s “low volume” alert—rehydrate and reassess.
9. Constipation and Hard, Dry Stools
Hydration affects stool moisture. If you’re dehydrated, the colon reabsorbs more water, producing harder stools that are painful or difficult to pass. While fluids aren’t a magic fix for every case, insufficient liquid intake is a recognized contributor—especially alongside low fiber and inactivity. If bowels have slowed and urine is dark, increase fluids (and fiber) and build a bathroom routine after meals. Seek care for alarm signs like blood in stool, fever, or weight loss.
9.1 How to fix it (two-part plan)
- Hydration: aim for steady sips through the day; soups and water-rich foods (fruit/veg) help.
- Fiber + movement: add 5–10 g/day of fiber (oats, beans, psyllium) and walk after meals.
9.2 Evidence snapshot
Low fluid intake is tied to higher constipation risk in epidemiology, and hydration helps when you’re actually hypohydrated; it’s less helpful if you’re already well-hydrated—so match fluids to your signs.
Bottom line: If stools are hard and infrequent—and your urine is dark—drink up, add fiber, and move.
10. Sunken Eyes, No Tears, or Few Wet Diapers (Infants & Children)
Pediatric dehydration can escalate quickly. In babies and young children, signs include sunken eyes, no tears when crying, a dry mouth, irritability or drowsiness, and fewer wet diapers. A sunken soft spot (fontanelle) is another red flag in infants. Vomiting/diarrhea are common triggers; use low-osmolarity ORS early and often, small sips or spoonfuls at a time. Seek urgent care if the child is very sleepy, has persistent vomiting, bloody stools, or hasn’t urinated for 6–8 hours (infant) or 8–12 hours (older child).
10.1 How to fix it (parent checklist)
- Start ORS immediately: 5–10 mL every 5 minutes, increasing as tolerated.
- Continue feeding: breast milk or usual formula; avoid sugary drinks/undiluted juice.
- Watch for danger: lethargy, sunken fontanelle, cold hands/feet, rapid breathing—get care.
10.2 Why ORS works
WHO/UNICEF recommend low-osmolarity ORS (~245 mOsm/L)—glucose helps the gut absorb sodium and water efficiently, cutting stool volume and IV needs. PubMed
Bottom line: In kids, act early with ORS and call the doctor sooner rather than later.
11. Heat Exhaustion: Nausea, Heavy Sweating, Clammy Skin (and When It’s Heat Stroke)
Dehydration is a core driver of heat exhaustion—marked by heavy sweating, weakness, nausea, dizziness, headache, and cool, clammy skin. Left unchecked, it can progress to heat stroke, a medical emergency with confusion, slurred speech, fainting, or hot, dry skin and core temperature ≥40°C/104°F. If you suspect heat stroke, call emergency services immediately, move to shade or AC, and start aggressive cooling (ice/cold packs to neck, armpits, groin; cold water immersion if trained and available). Do not delay care.
11.1 How to fix heat exhaustion (now)
- Cool first, rehydrate second: stop activity, shade/AC, cool packs; then sip ORS or water.
- Lay down with legs elevated; loosen clothing.
- Monitor: if symptoms don’t improve in 30 minutes or worsen, seek urgent care.
11.2 Prevention in hot climates (as of August 2025)
- Prehydrate: ~500 mL 2 hours before heat exposure; keep fluids handy.
- Work–rest cycles: schedule breaks in shade; use fans or evaporative cooling; wear light clothing.
- Know your signs: dizziness, cramps, or nausea in the heat mean stop and cool now. PubMed
Bottom line: In heat, treat dehydration early; know the red flags that require emergency action.
FAQs
1) What’s the fastest safe way to rehydrate?
Small, frequent sips of water or low-osmolarity ORS work best—especially after heavy sweating or GI illness. ORS contains sodium and glucose that speed water absorption in the small intestine; you’ll usually feel better within 15–60 minutes. If you’re vomiting, try 5–10 mL every 5 minutes and increase as tolerated. Call a clinician if you can’t keep fluids down.
2) Do coffee and tea count toward hydration?
Yes. Caffeinated beverages contribute to daily fluid intake; the mild diuretic effect is small for habitual drinkers. Prioritize water, milk, soups, and water-rich foods, and use electrolytes during prolonged sweating. Total daily fluid needs vary; many adults meet them around 3.7 L (men) and 2.7 L (women) from all beverages and foods.
3) How can I tell if I’m hydrated without buying gadgets?
Use the trio: urine color (aim for pale straw), thirst, and how you feel (energy, dizziness). For heat/exercise days, weigh yourself before and after; try to keep loss <2% body mass and replace what you lost over the next few hours.
4) When should I go to the ER for dehydration?
Go immediately for confusion, fainting, chest pain, a seizure, hot/dry skin with fever, or signs of heat stroke. For children: very sleepy, sunken eyes or fontanelle, no tears, or few/no wet diapers. IV fluids and evaluation may be needed.
5) What’s the difference between dehydration and overhydration (hyponatremia)?
Both can cause headache, nausea, and confusion. Overhydration dilutes blood sodium (hyponatremia), which can be dangerous in endurance events; it’s more likely if you drink only water for hours while sweating heavily. If you have symptoms and your urine is crystal-clear after heavy drinking, stop drinking plain water, rest, and seek medical care if symptoms persist. Use electrolytes during long, sweaty efforts.
6) Are “eight glasses a day” rules accurate?
They’re a rough starting point, not a rule. Needs shift with body size, heat/humidity, altitude, diet, pregnancy, and medications. Many adults fall near 3.7 L (men) / 2.7 L (women) total fluids including foods; let thirst, urine, and context guide you.
7) Which electrolyte mix is best?
For illness or heavy sweating, choose low-osmolarity ORS (WHO/UNICEF standard ~245 mOsm/L) or a sports drink with sodium. Avoid high-sugar sodas/juices during diarrhea—they can worsen stools. Read labels: ORS should contain sodium chloride, potassium chloride, trisodium citrate, and glucose.
8) Does dehydration affect mood and focus?
Yes. Even mild dehydration (≈1–2% body mass loss) can worsen mood and cognitive performance. Many people feel better within an hour of rehydrating and cooling down. The Journal of NutritionPMC
9) I’m older—am I at higher risk?
Older adults often have a diminished thirst response and may be on diuretics, both of which increase dehydration risk. Build routines: keep water visible, pair sips with medications/meals, and use soups and hydrating foods. Call a clinician earlier if you feel weak, dizzy, or confused. National Council on Aging
10) What about dehydration during Ramadan or intermittent fasting?
Plan your fluids strategically at non-fasting times: prioritize water, soups, milk, fruit, and ORS if you’re very active. Avoid very salty foods before fasting hours. Watch for dark urine and dizziness during daytime heat; reduce exertion and seek shade.
11) Can dehydration cause constipation even if I eat enough fiber?
Yes—low fluid intake is a recognized contributor. Fluids help fiber form soft, bulky stools. If you’re already well-hydrated, more fluid alone won’t fix constipation; combine fluids with fiber, movement, and bathroom routines. NIDDKPMC
12) Are urine color apps/strips worth it?
They can help some people, but you don’t need them. A simple paper urine color chart is validated; just compare a sample in a clear cup under good light. Pair with thirst and how you feel for best accuracy.
Conclusion
Your body is constantly signaling hydration status—through urine color and frequency, thirst, how your head feels, your energy, your skin, and your performance. When you learn to read those signals, you can fix most mild dehydration quickly: sip water or ORS, cool down, rest, and reassess within an hour. In hot weather or long workouts, plan ahead with prehydration and electrolytes, and keep body-mass loss under about 2%. For infants and older adults, act sooner and seek care earlier; dehydration escalates fast in these groups. Finally, remember that more isn’t always better—if you’re drinking for hours while sweating heavily, include sodium to avoid hyponatremia. Make hydration part of your routine—pair sips with meals, medications, meetings, or prayers—and treat urine color, thirst, and how you feel as your daily dashboard. Drink smart, cool down, and listen to your body.
CTA: Save this guide and set a reminder to check your “hydration dashboard” (urine–thirst–feel) three times tomorrow.
References
- Dehydration – Symptoms, causes, and treatment, Mayo Clinic, May 2, 2025. Mayo Clinic
- Water: How much should you drink every day?, Mayo Clinic, 2024–2025. Mayo Clinic
- Dehydration (Adults & Children), NHS Inform, Jan 10, 2025. NHS inform
- About Heat and Your Health, U.S. CDC, July 25, 2025. CDC
- Heat exhaustion: First aid, Mayo Clinic, 2025. Mayo Clinic
- Heat Cramps, Exhaustion, and Stroke—Signs & What to Do, National Weather Service, accessed 2025. National Weather Service
- Oral Rehydration Salts: Low-Osmolarity ORS (245 mOsm/L), WHO/UNICEF guidance, 2006 & updates. USAID Global Health Supply Chain Program
- Managing Acute Gastroenteritis Among Children, CDC MMWR, 2003. CDC
- Adult Dehydration, StatPearls/NCBI Bookshelf, updated 2022. NCBI
- Pediatric Dehydration, StatPearls/NCBI Bookshelf, updated 2024. NCBI
- Validation of urine color for assessing hydration, Frontiers in Nutrition, 2020. Frontiers
- Exercise-Associated Hyponatremia in Marathon Runners, Nutrients (PMC), 2022. PMC
- Water Intoxication (Hyponatremia), Cleveland Clinic, Sep 17, 2024. Cleveland Clinic
- Report Sets Dietary Intake Levels for Water, National Academies, Feb 11, 2004. National Academies
- American College of Sports Medicine Position Stand: Exercise and Fluid Replacement, Medline/PubMed, 2007. PubMed
- NHS 111 Wales: Dehydration—Signs in Adults, Children, and Babies, Jan 9, 2024. nhs.uk
- Good Hydration Linked to Healthy Aging, NIH/NHLBI, Jan 2, 2023. NHLBI, NIH
- Eating, Diet, & Nutrition for Constipation, NIDDK, 2025. NIDDK