A quick note before we start: this guide is for education, not personalized medical advice. If you have heart, bone, or metabolic conditions—or take medications that affect exercise—discuss any program with your clinician first.
Fitness goal planning for older adults means choosing age-appropriate, measurable targets that improve strength, balance, endurance, flexibility, and independence while managing risks. In practice, older adults generally do best with multicomponent programs: 150–300 minutes/week of moderate aerobic activity, muscle-strengthening 2+ days/week, and balance work several days/week—scaled to ability and health status. World Health Organization
1. Begin With Screening and Baselines (So You Can Train Safely)
Start by confirming it’s safe to exercise and by capturing a clear baseline; then your goals and progress will be meaningful. Most older adults can be active without extensive testing, but preparticipation screening helps identify who needs medical review first (e.g., new chest pain, unexplained dizziness, recent fall with injury). If you’re already active and symptom-free, you typically won’t need a stress test before moderate exercise, but anyone with concerning symptoms, complex cardiac history, or major mobility limits should speak with a clinician. Capture baselines like resting heart rate, blood pressure (if you monitor it), medications that may blunt heart-rate response (e.g., beta-blockers), simple functional tests (Timed Up and Go, 30-second Chair Stand), and a short mobility/balance self-rating. These numbers convert vague goals (“get fitter”) into objective targets and guardrails.
- Quick baseline kit
- Timed Up & Go (TUG): time to stand, walk 3 m/10 ft, return, sit. Many programs flag ≥12 seconds as elevated fall risk.
- 30-Second Chair Stand: total safe stands in 30 seconds (arms crossed).
- 6-Minute Walk: total distance walked at a steady pace.
- Subjective tools: Talk Test and RPE (0–10) to mark “easy/moderate/hard.”
1.1 Numbers & guardrails
- ACSM prescreening endorses simplified algorithms that reduce unnecessary barriers; symptoms and disease history guide when to seek medical clearance. Exercise is Medicine
- TUG: many clinical resources use ≥12 seconds as a risk flag; use as a trend, not a diagnosis.
- Chair Stand and 6-Minute Walk have standardized protocols—use the same set-up each time.
Bottom line: screen for red flags, record a few simple baselines, and use them to personalize pace and monitor improvement—not to exclude yourself from moving.
2. Define “Better” as Function First (Independence, Not Just Aesthetics)
For older adults, the most powerful goals are function-first: standing up from a chair effortlessly, carrying groceries, climbing stairs without knee pain, stepping off a curb without wobbling, walking 30–45 minutes comfortably, or playing with grandkids. Tie each function to a metric and a behavior plan. For example, “Rise from any standard chair without using hands within 8 weeks” paired with 3 sets of sit-to-stands, three days per week. Similarly, “Walk briskly for 30 minutes without stopping” pairs well with an interval-style walking plan and weekly distance checks. Functional goals feel relevant (daily life), adaptive (scale up or down), and protective (they reduce fall and hospitalization risk).
- Examples of function-first outcomes
- Sit-to-stand power: chair stands improve leg strength and balance.
- Gait endurance: six-minute walk distance and everyday step counts.
- Reactive balance: tandem stance/single-leg stance progression.
- Floor recovery: safe kneel-to-stand sequence practice.
2.1 Mini-checklist
- Does the goal improve ADLs (activities of daily living)?
- Is there a clear metric (time, distance, reps, seconds of balance)?
- Is the plan behavior-linked (which days, how many sets, how long)?
- Is there built-in review (every 2–4 weeks, repeat the same tests)?
Bottom line: anchor everything to everyday capability; body composition changes can follow, but independence and confidence come first.
3. Use SMART, Age-Smart Goals (Specific, Measurable, Able, Relevant, Time-Bound)
SMART still works—just make it age-smart. “Walk more” becomes “On Monday/Wednesday/Saturday, walk 22 minutes at a pace where I can talk but not sing.” “Get stronger” becomes “On Tuesday/Friday, perform 8–10 resistance exercises (bands, dumbbells, bodyweight) for 1–2 sets of 8–12 reps at RPE 5–7.” Make goals Able (safe with your conditions), Relevant (to your life), and time-bound (2, 4, 8-week checkpoints). Use RPE 0–10 and the Talk Test to set intensity without relying on gadgets or heart-rate formulas, which can mislead if you take beta-blockers.
- SMART template you can copy
- S: “TUG under 12 seconds” or “walk 2 km without stops.”
- M: Weeks with ≥150 minutes moderate activity + 2 strength days.
- A: Doctor/physio cleared; no symptom triggers.
- R: Improves balance, stamina, or pain-free range needed for daily life.
- T: Re-test in 4 weeks; adjust sets/reps/time by 5–10%.
3.1 Why RPE & Talk Test?
CDC and clinical sources endorse the Talk Test and perceived exertion (RPE 5–6 = moderate; 7–8 = vigorous) as practical intensity guides, especially when heart-rate targets are unreliable.
Bottom line: make the plan concrete and check progress on a schedule; use simple intensity tools that work with (not against) your medications and energy levels.
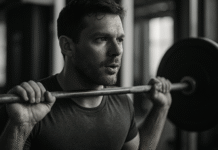
4. Prioritize Strength Training 2–3 Days/Week (Muscle Is Mobility Insurance)
Strength work is the highest-leverage investment for older adults. It fights sarcopenia (age-related muscle loss), improves bone loading, powers sit-to-stands and stair climbing, and supports glucose control. Aim for 2–3 non-consecutive days/week, training all major muscle groups with 1–3 sets of 8–12 controlled reps at RPE 5–7 (a “somewhat hard” effort where you could do 2–3 more reps). Use machines, dumbbells, kettlebells, or resistance bands. Start with large-range, low-load movements and progress load or difficulty by 5–10% when you complete the top end of reps comfortably. Include some power (fast-up, slow-down) drills like controlled sit-to-stands and step-ups to maintain the ability to react and prevent stumbles.
- Starter menu (pick 6–8)
- Sit-to-stand, hip hinge (hip-dominant), step-ups, supported split squat
- Row/pulldown, chest press/wall push-ups, overhead press (as tolerated)
- Heel raises, marches, side-steps with a band, farmer’s carry
4.1 Common mistakes
- Only doing cardio—skip that and you miss the “strength to use your endurance.”
- Holding your breath; use a gentle exhale on exertion.
- Chasing soreness; progress gradually instead.
Bottom line: strength training protects independence; start light, stay consistent, and let form and RPE guide the load.
5. Make Balance a Weekly Priority (3+ Days/Week) to Cut Fall Risk
Falls are the leading cause of injury in older adults, and balance training works. Plan 3+ short sessions/week of static and dynamic balance: tandem stance, single-leg stance near support, heel-to-toe walking, weight shifts, and turning drills. Layer in Tai Chi or a physical-therapist-led Otago program for proven fall-reduction benefits. Progress by reducing hand support, narrowing stance, closing eyes (with supervision), or adding light head turns. Keep sessions brief (10–20 minutes) and frequent.
- Evidence-based options
- Tai Chi: meta-analyses show reduced fall risk and fewer falls.
- Otago Exercise Program: structured home-based strength and balance program with demonstrated fall-reduction.
5.1 Mini-checklist
- Practice near a stable support (counter, sturdy chair).
- Shoes: supportive, non-slip soles; check foot issues that alter balance.
- Re-test with TUG or a simple tandem stand (≥10 seconds target). CDC
Bottom line: short, regular balance work prevents injuries that derail progress; make it a standing appointment, not an afterthought.
6. Program Aerobic Conditioning You’ll Keep (150–300 Min/Week, Any Bouts)
Older adults benefit from 150–300 minutes/week of moderate aerobic activity (brisk walking, cycling, swimming) or 75–150 minutes vigorous, or a combination. As of December 2023, guidelines emphasize that any bout length counts—2–5 minute “movement snacks” add up. Use the Talk Test (talk but don’t sing) to stay in the moderate zone. If starting from low activity or multiple conditions, build toward 10–15 minutes/session, adding 2–5 minutes every week as tolerated. Intervals are fine: e.g., 2 minutes brisk / 1 minute easy repeated 6–10 times.
6.1 Numbers & options
- Begin with 22 minutes/day (or two 11-minute walks) to reach 150 min/week.
- If heat or air quality is high (common in many regions), walk early, indoors, or at malls; hydrate and use shaded routes.
- For joint pain, try water walking or a recumbent bike.
Bottom line: pick the most sustainable cardio option, track total weekly minutes, and add a little over time—consistency beats intensity.
7. Protect Bones and Joints With Osteoporosis-Smart Modifications
If you have osteoporosis or are at high fracture risk, stay active—exercise is part of treatment—but move strategically. Emphasize upright, weight-bearing activity (walking, stair steps, gentle impact if appropriate) and resistance training for hips, legs, and spinal extensor muscles. Many guidelines recommend avoiding deep, loaded spinal flexion and forceful twisting, especially after vertebral fracture; prioritize neutral-spine hip hinges, supported rows, and posture drills. Balance training is essential. If you’re unsure about specific movements (e.g., crunches, toe-touches), ask a physio trained in osteoporosis-safe exercise.
- Safer substitutions
- Swap sit-ups for bird-dogs or wall planks.
- Practice hip hinge with dowel (three points of contact) before deadlifts.
- Build postural endurance with prone back extensions and chest-openers. International Osteoporosis Foundation
7.1 Region-specific note
Where sidewalks are uneven or lighting is poor, favor indoor circuits (hallway walks, step-ups, balance near a countertop) and daylight outings; consider a walking pole for extra stability.
Bottom line: maintain bone-friendly loading while avoiding high-risk spinal positions; “move more, but move wisely.”
8. Flexibility and Mobility: Gentle, Daily, and Purpose-Built
Flexibility keeps joints comfortable and posture efficient—but it’s the right kind that matters. Favor dynamic warm-ups before activity (leg swings, shoulder circles) and gentle static stretches after muscles are warm. Keep each stretch 15–30 seconds, 2–4 times, with no pain or bouncing. Target areas that limit your function: calf-ankle for walking, hip flexors for upright posture, thoracic rotation for turning, and chest/shoulder for reach. If you have osteoporosis, avoid end-range spinal flexion; choose chest-openers and hip-hinge mobility instead. Mayo Clinic
8.1 Mini-sequence (8–10 minutes)
- Ankle rocks → calf stretch → hip flexor lunge at counter
- Thoracic open-books (side-lying) → chest doorway stretch
- Seated hamstring stretch (neutral spine) → scapular retraction holds
Bottom line: stretch what’s tight because it limits life, not to chase arbitrary range; keep it warm, gentle, and spine-smart.
9. Recover Like It’s Part of Training (Because It Is)
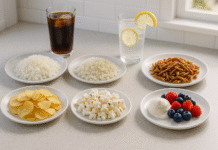
Progress happens between sessions. Plan at least 48 hours between heavy strength days, sleep 7–9 hours/night, hydrate, and include light movement on “off” days (walks, mobility, Tai Chi). If you’re on medications (e.g., beta-blockers) that alter HR, lean on RPE and the Talk Test to regulate intensity. Muscle soreness is normal early on; joint pain, chest pain, or dizziness are not—scale back and seek guidance. Nutrition matters: many expert groups suggest older adults target ~1.0–1.2 g of protein/kg/day (higher—up to 1.5 g/kg—when ill or in rehab, unless contraindicated). Spread protein across meals (20–35 g/meal) to stimulate muscle protein synthesis.
9.1 Mini-checklist
- Repeat the same lifts only after joints feel normal.
- If morning stiffness > 60 minutes after new exercises, reduce volume next time by 20–30%.
- On hot days, pre-hydrate and consider indoor sessions.
Bottom line: schedule recovery like a workout—sleep, protein, hydration, light movement—and your progress accelerates safely.
10. Track What Matters (Simple Tests, Clear Logs, Regular Reviews)
What gets measured gets improved. Re-test every 4–6 weeks with the same protocols and record your results in a notebook or app. Track training minutes, strength sets/reps at RPE, balance durations, and functional test scores (TUG, Chair Stand, 6-Minute Walk). Celebrate improvements like “TUG 14.2 → 11.9 seconds,” “Chair Stands 9 → 13,” or “Walk distance 380 m → 470 m.” Use small plateaus to adjust: if progress stalls, add a set, tweak exercise order, or vary walking routes.
- Reference protocols
- Chair Stand (CDC STEADI one-pager).
- Six-Minute Walk (ATS protocol).
10.1 Tools/Examples
- Paper log, spreadsheet, or a basic habit-tracker app.
- Phone reminders for balance “snacks” at 10 a.m. and 4 p.m.
- Pedometer/step counter for simple daily movement nudges.
Bottom line: keep tracking simple and repeatable; small, steady upticks compound into big functional wins.
11. Build Safety Signals Into Every Session (Know When to Stop)
Safety isn’t passive; make it procedural. Warm up 5–10 minutes, check how you feel today (RPE “body scan”), and set a session goal. During training, use RPE 5–6 for most sets and the Talk Test for cardio. Stop and reassess if you feel chest pressure, unusual shortness of breath, dizziness, or joint pain that alters your movement. If you’re on beta-blockers or similar medications that blunt heart-rate response, prioritize RPE and symptom checks; HR may under-represent effort. PubMed
11.1 Mini-checklist
- Environment: good lighting, clear floor, stable footwear.
- Progressions: change one variable at a time (load or reps or support).
- Cool-down: 3–5 minutes easy walking + gentle stretches.
Bottom line: a few consistent safety rituals dramatically reduce setbacks; they also build confidence, which keeps you moving.
12. Make It Social and Habit-Friendly (Because Motivation Loves Company)
Adherence drives outcomes. Pair sessions with existing routines (habit stacking): after breakfast, 10–15 minutes of mobility; after afternoon tea, a 20-minute walk; Tuesday/Friday mornings, strength and balance. Join a group class (walking club, Tai Chi, water aerobics) for accountability and fun. Design your space (bands by the chair, sturdy counter space for balance, filled water bottle ready). Keep a short “fallback workout” for busy days (two sets of sit-to-stands, wall push-ups, rows, heel raises, and a short walk). Celebrate process milestones (10 workouts in a month) as much as results.
12.1 Evidence-backed options
- Community Tai Chi classes and STEADI fall-prevention resources offer structure and social support. CDC
Bottom line: make the plan easy to start, obvious to continue, and enjoyable with people; consistency is the strongest medicine.
FAQs
1) What’s the best weekly exercise mix for adults 65+?
Aim for 150–300 minutes of moderate cardio, 2+ strength days, and frequent balance practice. If you’re rebuilding from very low activity or several conditions, start smaller (even 5–10 minute bouts) and build. Any movement is better than none, and short bouts count as of late-2023 guidelines.
2) How hard should my workouts feel?
Use the Talk Test and RPE 0–10. Moderate feels like RPE 5–6—you can talk, not sing. Vigorous is 7–8—speaking full sentences is tough. These tools are reliable, especially if your medication blunts heart rate. CDC
3) I have osteoporosis—can I still lift?
Yes—exercise is encouraged. Focus on resistance training for hips and back extensors, walking/impact (as appropriate), and balance. Many consensus statements caution against deep, loaded spinal flexion and forceful twists, especially after vertebral fractures. A physio can tailor your plan.
4) Which simple tests should I repeat to see progress?
Good choices: Timed Up & Go (aim <12 seconds), 30-Second Chair Stand, 6-Minute Walk distance, and simple balance holds (tandem/single-leg). Use consistent conditions each time.
5) Is walking enough?
Walking is excellent for heart health and mood, but you’ll miss key benefits without strength and balance work. A multicomponent program reduces fall risk and preserves independence.
6) What about protein—do older adults need more?
Many expert groups advise ~1.0–1.2 g/kg/day, with 1.2–1.5 g/kg when ill or in rehab (unless your clinician says otherwise). Distribute protein across meals (20–35 g each). PMC
7) Can Tai Chi or Otago really prevent falls?
Yes—Tai Chi and the Otago Exercise Program have evidence for reducing falls and improving balance. Consider them if you’re unsteady or have fallen in the past year. PubMedUNC School of Medicine
8) My heart-rate monitor shows low numbers on meds—is that okay?
Beta-blockers lower heart rate at rest and during exercise; HR targets may mislead. Use RPE, the Talk Test, and your clinician’s guidance (especially if you had a recent stress test). PMC
9) How do I progress without getting sore or injured?
Increase one variable at a time by 5–10% (more reps or slightly more load or less support). Keep RPE in the 5–7 range for strength. If soreness lasts >48 hours or alters your walk, scale back.
10) What if I can’t hit 150 minutes/week yet?
Do what you can—and accumulate minutes. Two to four 5- to 10-minute bouts/day add up. The key is consistency, not perfection. CDC
Conclusion
For older adults, the smartest fitness goals are function-first, measurable, and habit-friendly—and they’re anchored by three pillars: strength (your mobility insurance), balance (your fall-prevention shield), and aerobic conditioning (your energy and heart health). Start with screening and simple baselines, define “better” as independence you can feel, then build a week around 2–3 strength days, frequent balance snacks, and sustainable cardio minutes. Use RPE and the Talk Test to dial intensity, and treat recovery (sleep, hydration, protein) as non-negotiable training sessions. Re-test every month, make small adjustments, and recruit social support to stay on track. The result isn’t just fitness—it’s confidence in your body, fewer stumbles, and more of the life you want to live.
Copy-ready CTA: Start today with 10 minutes of balance, a brisk 15-minute walk, and 2 sets of sit-to-stands—then add a little each week.
References
- Older Adult Activity: An Overview — Centers for Disease Control and Prevention (CDC). Dec 22, 2023. CDC
- Physical Activity Guidelines for Americans, 2nd ed. — U.S. Department of Health and Human Services (ODPHP). 2018. Health.gov
- WHO Guidelines on Physical Activity and Sedentary Behaviour — World Health Organization. Nov 25, 2020. WHO IRIS
- Applying the ACSM Preparticipation Screening Algorithm — Current Sports Medicine Reports. 2017. PMC
- Assessment: Timed Up & Go (TUG) — CDC STEADI. 2024. CDC
- Assessment: 30-Second Chair Stand — CDC STEADI. 2024. CDC
- ATS Statement: Guidelines for the Six-Minute Walk Test — American Thoracic Society. 2002. American Thoracic Society
- Strong, Steady and Straight: UK Consensus on Physical Activity and Osteoporosis — Osteoporosis International. 2022. PMC
- Evidence-Based Recommendations for Optimal Dietary Protein Intake in Older People (PROT-AGE) — JAMDA. 2013. PubMed
- ESPEN Practical Guideline: Clinical Nutrition and Hydration in Geriatrics — Clinical Nutrition. 2022. Clinical Nutrition Journal
- What You Can Do To Prevent Falls — CDC STEADI Brochure. Feb 2025. CDC
- Tai Chi for Fall Prevention in Older Adults: Meta-analysis of RCTs — (example) Frontiers in Medicine, 2024. Frontiers